Embarking on the intricate journey of healthcare, a Patient Consent Form stands as a pivotal beacon, illuminating the path of medical ethics and patient rights. Navigating through its meanings, various types, and quintessential examples, we’ll delve into the nuances that safeguard both practitioners and patients alike. This guide will elucidate not only its foundational importance but also provide a step-by-step path on its creation, intertwined with practical tips to enhance its efficacy and comprehensibility in the ever-evolving healthcare landscape.
What is a Patient Consent Form? – Definition
A Patient Consent Form is a legal document that seeks a patient’s explicit permission before conducting specific medical interventions, procedures, or handling of their personal and health-related data. These fillable form ensures that the patient is adequately informed about the risks, benefits, and alternatives related to a proposed treatment or procedure. The fundamental essence of a Patient Consent Form lies in upholding the ethical principle of patient autonomy, ensuring that individuals have full control over what happens to their bodies and personal information within the healthcare domain.
What is the Meaning of the Patient Consent Form?
The Patient Consent Form symbolizes an ethical and legal acknowledgement, reflecting an individual’s autonomous decision to permit specific medical actions by healthcare professionals. It means that the patient has been duly informed about, understands, and agrees to the impending procedures, treatments, or data handling, ensuring their autonomy and rights are respected. The essence of the form is not merely in the authorization of medical actions but in substantiating that the patient’s decision is made with thorough awareness and devoid of coercion. This adherence to informed consent underpins ethical medical practice and safeguards patient well-being and autonomy.
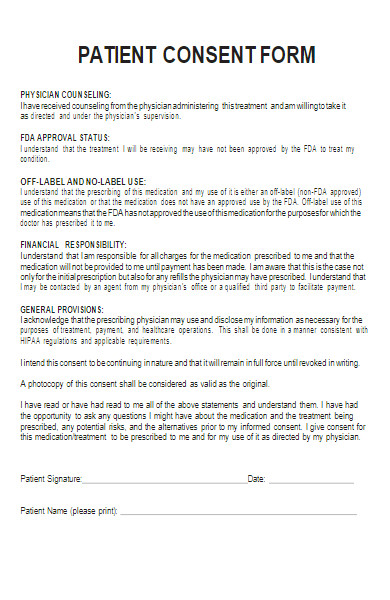
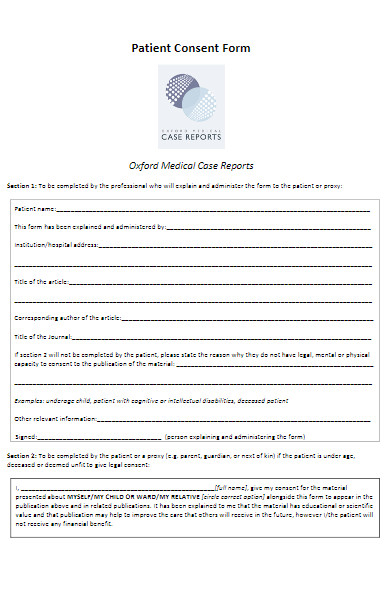
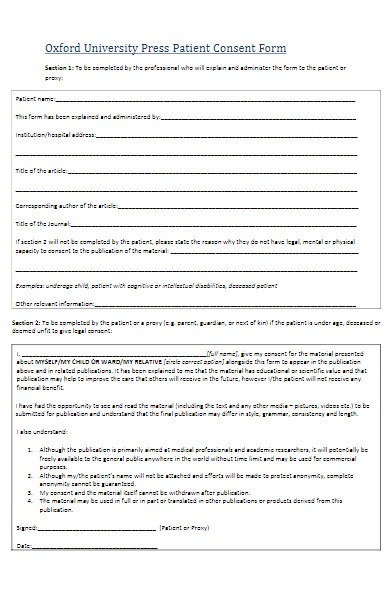
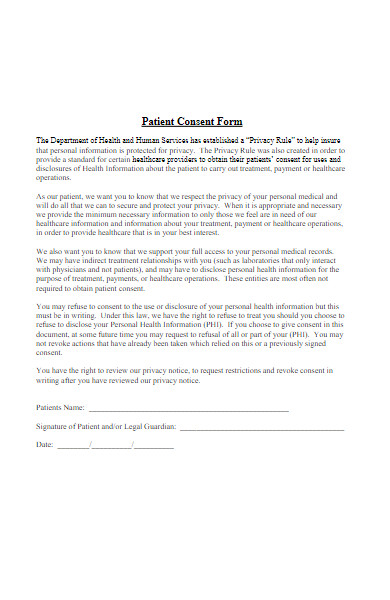
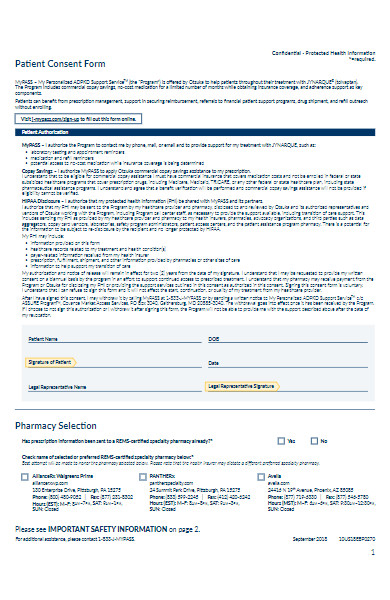
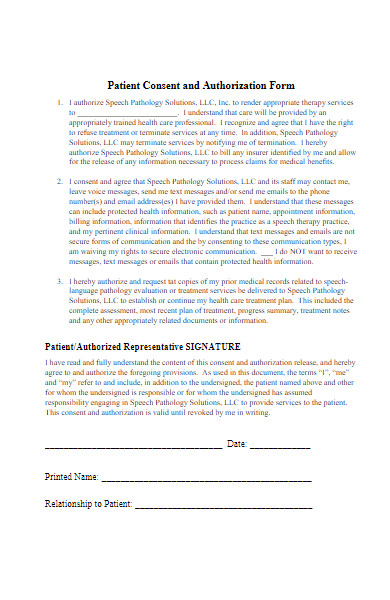
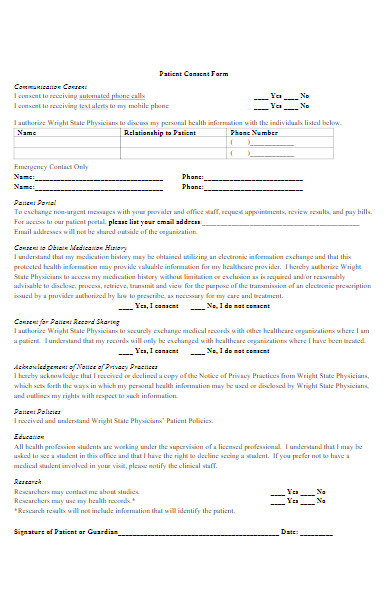
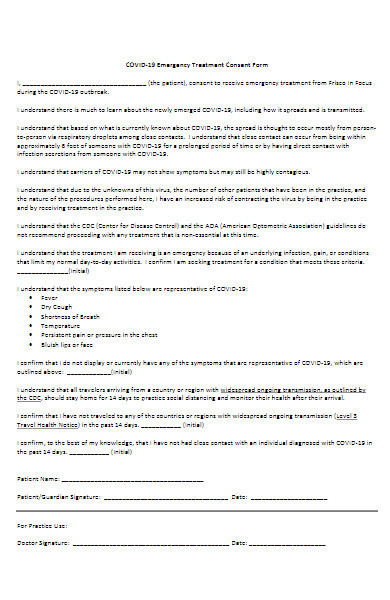
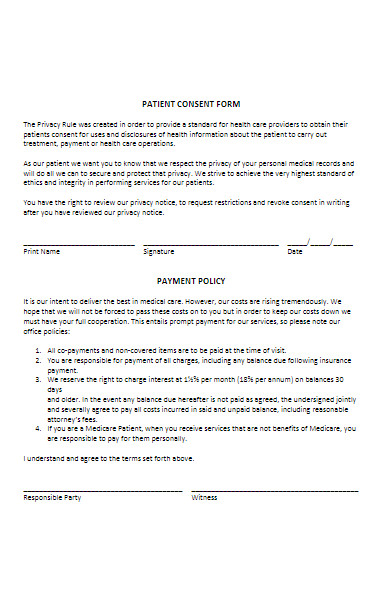
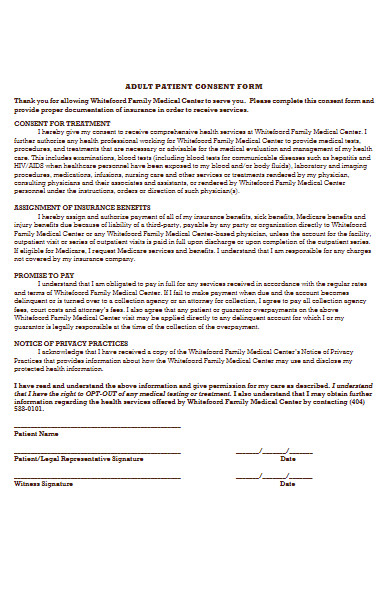
What is the Best Sample Patient Consent Form?
Creating the best sample Patient Consent Form necessitates a balance between legal, ethical, and patient-friendly communication. Though specific contents might vary per jurisdiction and medical specialty, a universally robust Patient Consent Form should be comprehensive, clear, and cater to the specific context of the treatment or procedure. Here’s a breakdown:
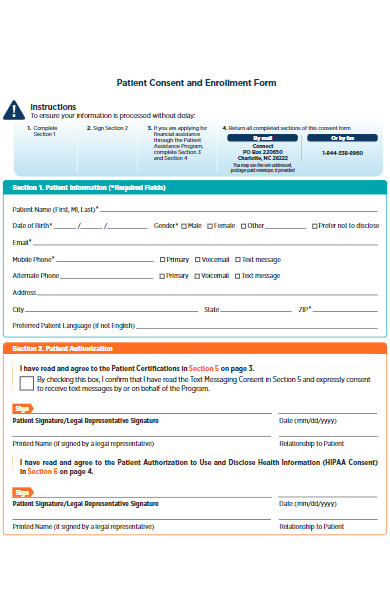
Header Information:
- Title: Clearly labeled as “Patient Consent Form”.
- Date: To validate its timeliness.
- Healthcare Provider Details: Name, qualification, and contact information.
- Patient Details: Full name, date of birth, and contact information.
Procedure Information:
- Description: A detailed account of the proposed medical procedure or treatment.
- Purpose: The intended medical benefit or outcome.
- Risks and Alternatives: Comprehensive details of potential risks and alternative options.
Consent Section:
- Informed Consent Statement: A declaration that information has been understood and all queries have been addressed.
- Voluntary Participation: A statement ensuring that the patient is participating without coercion.
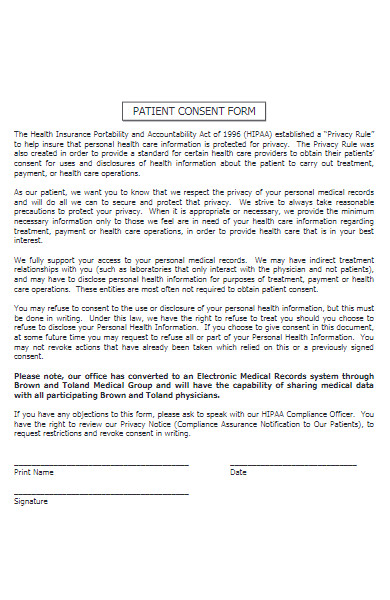
Privacy and Data Handling:
- Data Usage: How patient data will be used and stored.
- Privacy Assurance: Ensuring adherence to data protection regulations.
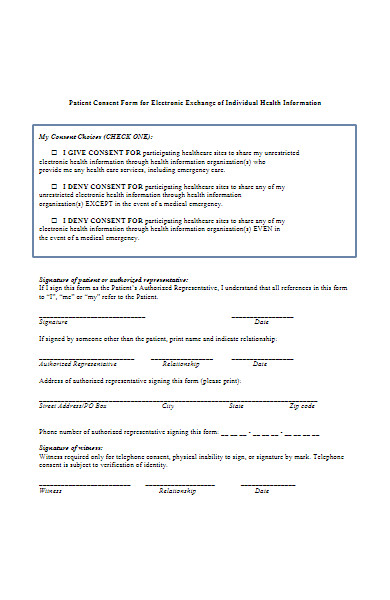
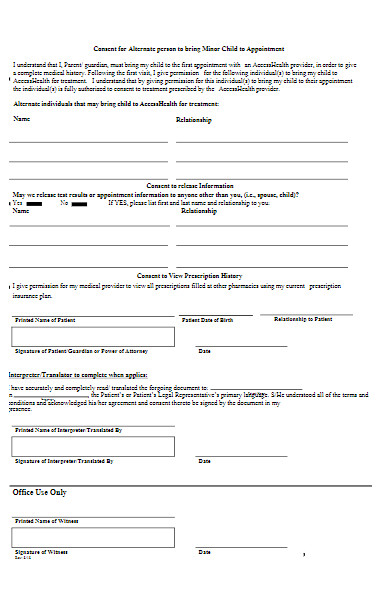
Signature Section:
- Patient’s Signature: A line for the patient to sign and date, confirming their consent.
- Witness Signature: To validate the patient’s signature, where applicable.
- Practitioner’s Signature: Validating that the patient has been appropriately informed.
Additional Components:
- Emergency Contact: Information about the patient’s emergency contact.
- Language and Understanding Assurance: Confirming that the patient comprehends the provided information.
- Special Considerations: Any unique patient-specific data or requirements.
Optional but Recommended:
- Revocation Clause: Details on how and under what conditions the patient may withdraw consent.
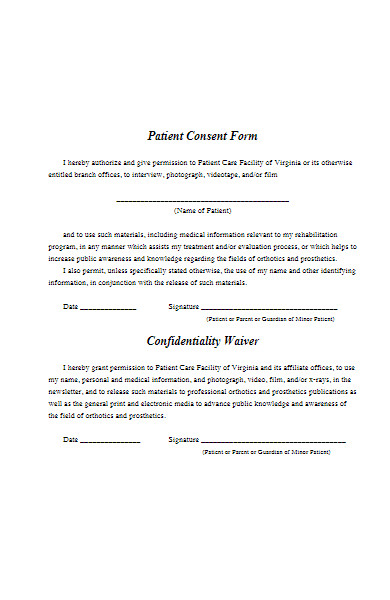
- Photographs or Videos: If any visual documentation will be taken and how it will be used.
Footer:
- Document Revision Date: To ensure the form’s most recent version is being utilized.
Notes for Creation:
- Language Clarity: The form must be in simple, easy-to-understand language.
- Legal and Ethical Adherence: Ensure it complies with regional laws and ethical guidelines.
- Accessibility: Should cater to varied linguistic and disability needs.
Final thoughts: Always consult a healthcare attorney or a professional specializing in medical law and ethics to ensure the Patient Consent Form aligns with all applicable legal and ethical norms. This detailed breakdown provides a generalized guide, but specific nuances may be necessary depending on local laws and the particular medical context. You should also take a look at our Sample Informed Consent Forms.
FREE 50+ Patient Consent Forms in PDF
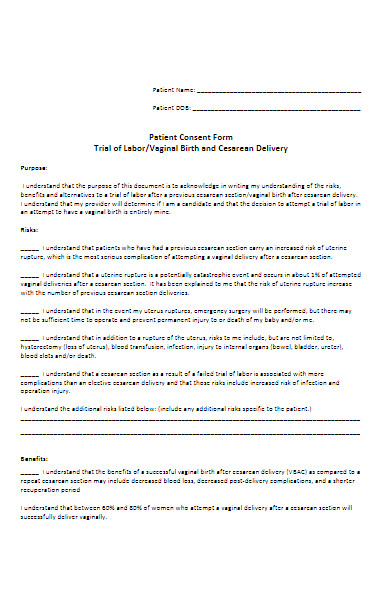
51. Labor Patient Consent Form
How do you write a patient consent form?
Creating a Patient Consent Form involves a meticulous process that adheres to both ethical guidelines and legal requirements. Ensuring clarity and comprehensive information is paramount to uphold patient autonomy and informed consent. Here’s a simplified guide to drafting a Patient Consent Form:
1. Basic Details
- Title: Indicate clearly at the top that the document is a “Patient Consent Form.”
- Patient Details: Include name, date of birth, and other relevant identification details.
- Provider Details: Mention the healthcare provider’s name, qualification, and contact info.
2. Procedure Information
- Detailed Description: Explain the procedure or treatment in straightforward language.
- Purpose: Describe the intended benefits and expected outcomes.
- Potential Risks: Detail possible adverse effects and associated risks.
- Alternatives: Present alternative procedures or treatments available.
3. Consent Statement
- Informed Consent Assurance: Declare that all provided information has been understood and all queries have been resolved.
- Voluntariness Affirmation: Confirm the patient’s consent is voluntary and uncoerced.
4. Privacy Assurance
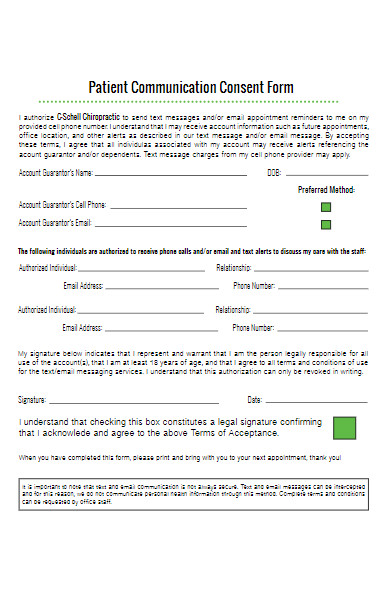
- Data Protection: Describe how the patient’s information will be stored and used.
- Confidentiality: Ensure that patient data will be kept confidential, specifying any circumstances under which it may be disclosed.
5. Right to Withdraw
- Explain Withdrawal: Detail how a patient can withdraw consent and any pertinent timelines or procedures.
- Implications: Mention any consequences or follow-up actions upon withdrawal.
6. Emergency Contact
- Contact Details: Include a section for the patient to provide an emergency contact person and their details.
7. Signature Section
- Patient’s Signature: Spaces for the patient to affirm their understanding and consent.
- Provider’s Signature: Verification from the healthcare professional that they’ve explained and answered all of the patient’s questions.
- Witness’ Signature: If applicable, for additional verification.
8. Miscellaneous
- Special Considerations: Address any patient-specific needs or requests.
- Additional Notes: A space for any pertinent notes or additional information.
- Glossary: Consider including a section that defines any technical terms.
9. Legal Compliance
- Ensure that the form adheres to regional and international laws regarding patient consent and data protection, like HIPAA in the USA or GDPR in Europe.
10. Accessibility
- Make sure the form is accessible and available in different languages or formats as per the patient’s needs.
Additional Tips:
- Use Simple Language: Ensure that medical jargon is minimized or adequately explained.
- Be Transparent: All potential outcomes, risks, and alternatives should be openly disclosed.
- Legal Consultation: Always have the form reviewed by a legal expert specialized in healthcare.
This guide provides a foundation for creating a Patient Consent Form format, but always consider healthcare-specific norms, legal requirements, and ethical considerations for comprehensive and compliant documentation.
What Information Should be Included in a Patient Consent Form?
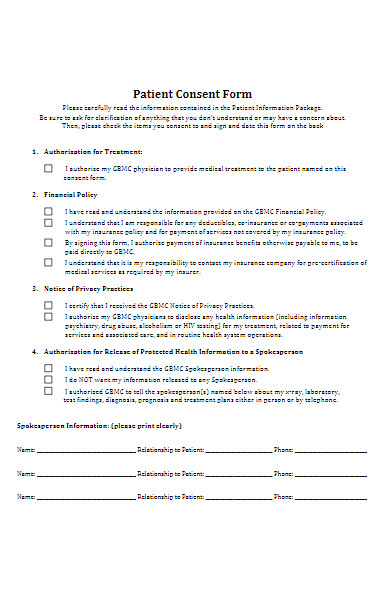
A Patient Consent Form should be a well-structured document that covers all aspects of the medical procedure and protects both the healthcare provider and the patient’s rights. The following components are typically included to ensure the consent is informed, voluntary, and comprehensive:
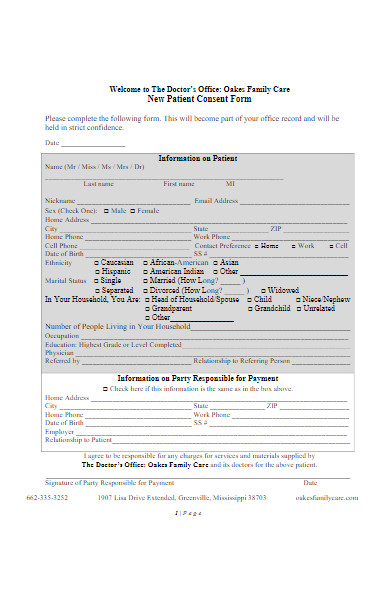
1. Patient Information
- Full name
- Date of birth
- Contact details
2. Healthcare Provider Information
- Practitioner’s name
- Credentials and specialty
- Contact details
3. Detailed Procedure Information
- Name and description of the procedure or treatment
- Purpose and expected benefits
- Potential risks and discomforts
- Alternatives available and their respective risks
- What will happen if the treatment is not pursued
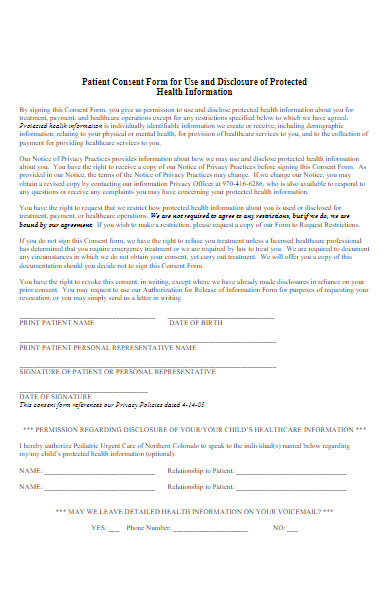
4. Consent Statement
- A clear statement indicating that the patient understands the information and agrees to proceed
- Assurance of voluntariness
- Mention that the consent can be withdrawn at any time
5. Data Privacy and Confidentiality
- How the patient’s data will be used and protected
- Situations in which information might be shared and with whom
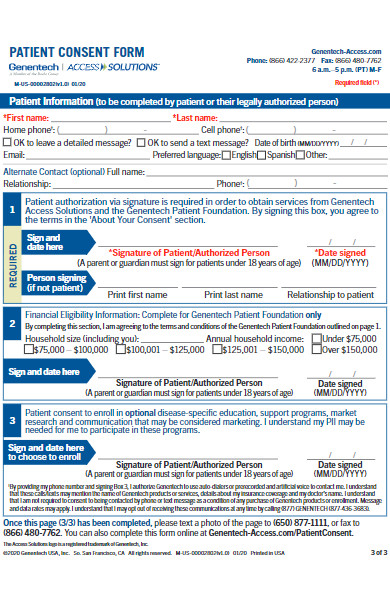
6. Financial Implications
- Costs associated with the procedure
- Payment methods and plans
7. Risks and Complications
- Potential side effects and complications
- Likelihood of success
- Quality of life post-procedure
8. Post-Procedure Care
- Expected recovery time
- Aftercare and rehabilitation
- Follow-up appointments and ongoing management
9. Emergency Contact
- Space for patient to fill in an emergency contact person and details
10. Signature Section
- Space for the patient to confirm understanding and agreement
- Practitioner’s signature validating accurate information provision and answering of questions
- Date to validate timeliness
11. Right to Withdraw Consent
- Explanation about the right to withdraw consent
- Process to withdraw and any related implications
12. Additional Clauses (if relevant)
- Clauses related to photography, video recording, or using patient data for research or educational purposes
- Any other specific clauses relevant to the healthcare provider or procedure
Additional Notes
- Ensure the language is easy to comprehend
- If possible, translate into relevant languages to cater to a diverse patient base
- Verify that it aligns with legal and ethical guidelines pertinent to the jurisdiction
The primary goal of a Patient Consent Form is to safeguard the patient’s rights, maintain transparency, and protect healthcare providers by ensuring all relevant information has been disclosed, and consent has been knowingly and willingly provided.
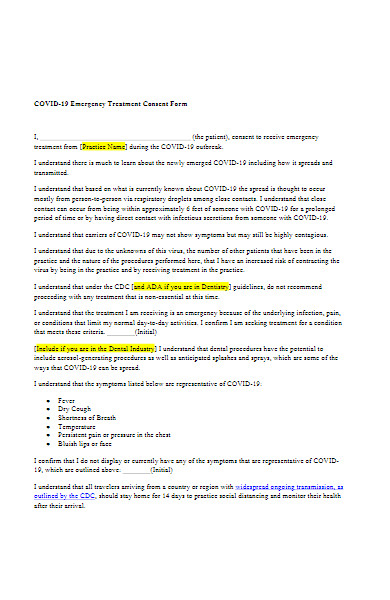
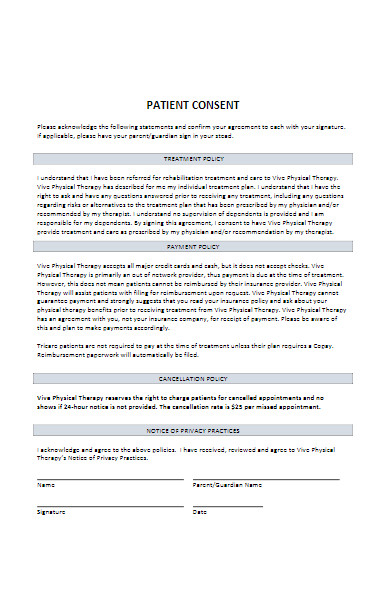
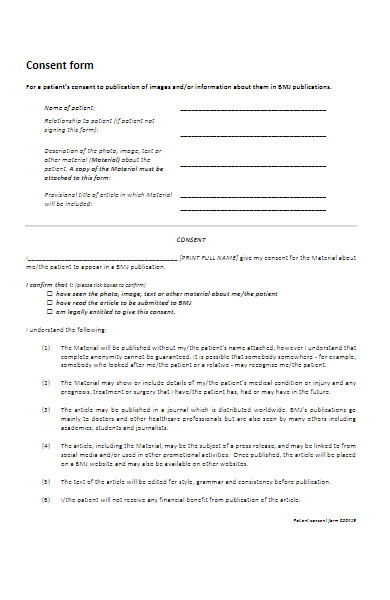
What are the Different Types of Patient Consent Forms?
Patient consent forms are essential in healthcare to ensure that patients are informed and their rights are respected. Different medical situations and purposes call for different types of consent forms samples. Here are some common types of patient consent forms used in healthcare settings:
1. Informed Consent Form
- Purpose: To obtain permission for medical treatments, procedures, or participation in clinical trials.
- Key Elements: Detailed information about the treatment, alternatives, risks, and benefits.
2. Implied Consent Form
- Purpose: Used when consent is not explicitly provided by the patient but is nonetheless inferred from their actions.
- Key Elements: Not applicable as the consent is not written but understood from the context (like extending an arm for a blood test).
3. Express Consent Form
- Purpose: For scenarios where explicit consent is necessary and is given through clear verbal or written communication.
- Key Elements: Clear statement of agreement to the proposed medical intervention.
4. Surgical Consent Form
- Purpose: To obtain permission for surgical procedures.
- Key Elements: Details of the surgery, surgeon, risks, benefits, alternatives, and possible complications.
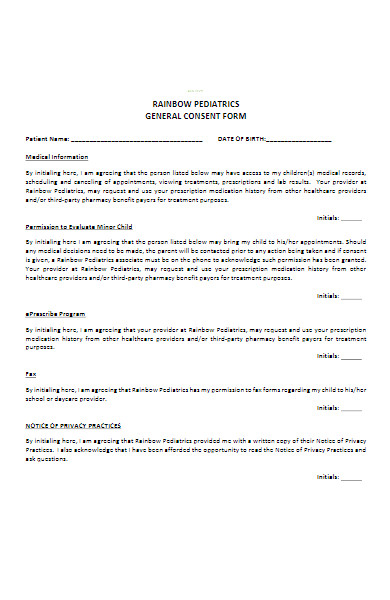
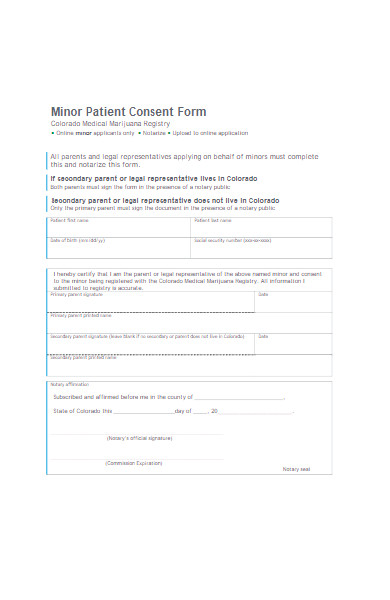
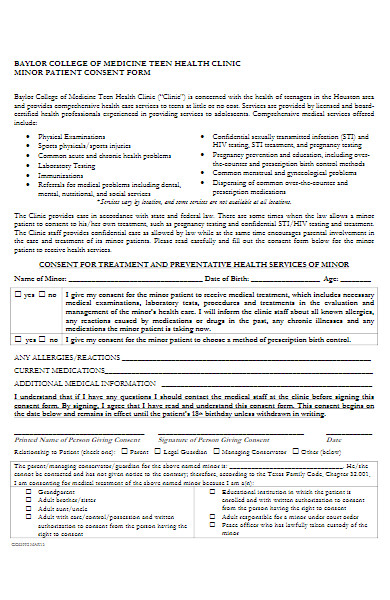
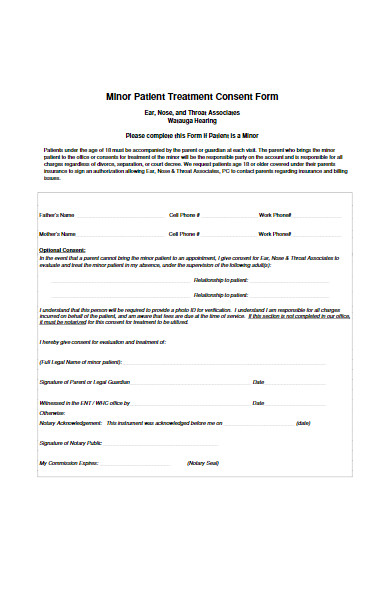
5. Child Medical Consent Form
- Purpose: To authorize a minor’s medical treatment when the parent or guardian is not present.
- Key Elements: Details about the child, the guardian, and the specific medical interventions allowed.
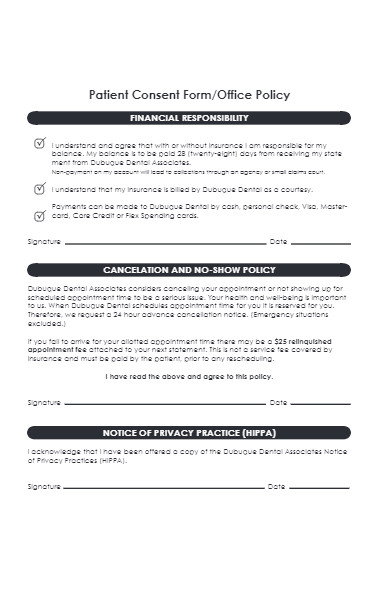
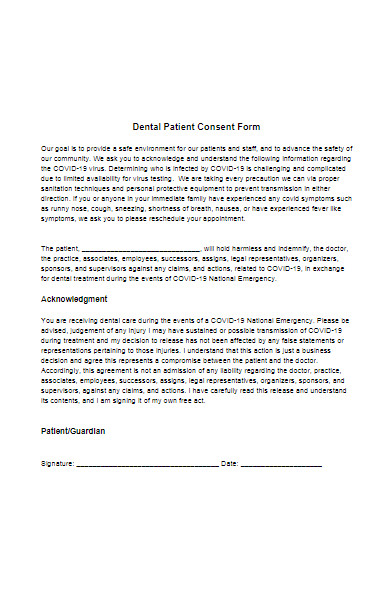
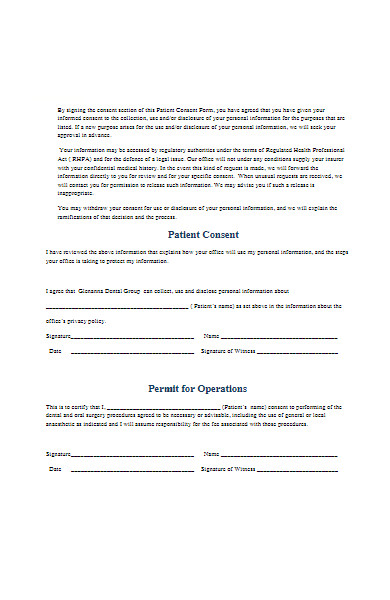
6. Dental Consent Form
- Purpose: To approve dental surgeries, treatments, or procedures.
- Key Elements: Details of the dental procedure, dentist, potential risks, and alternative treatments.
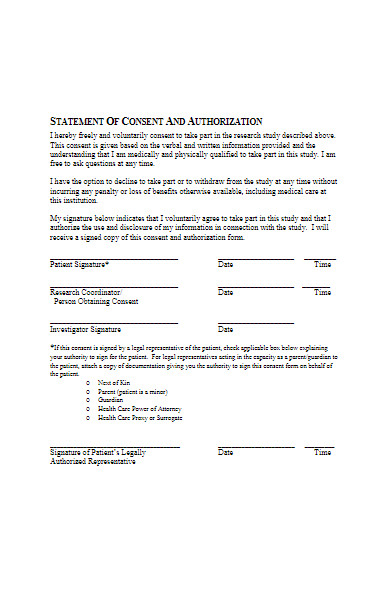
7. Research Consent Form
- Purpose: To gain approval for participation in medical or healthcare-related research.
- Key Elements: Project details, risks, benefits, confidentiality assurances, and participant rights.
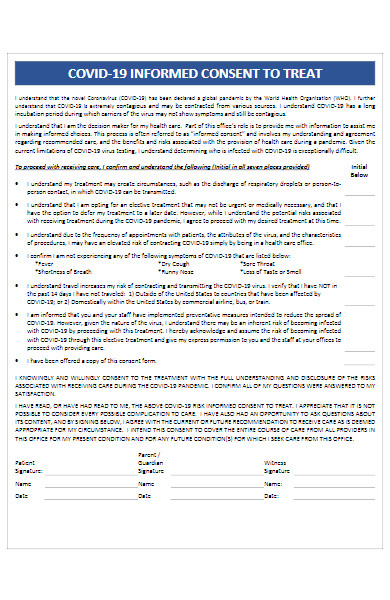
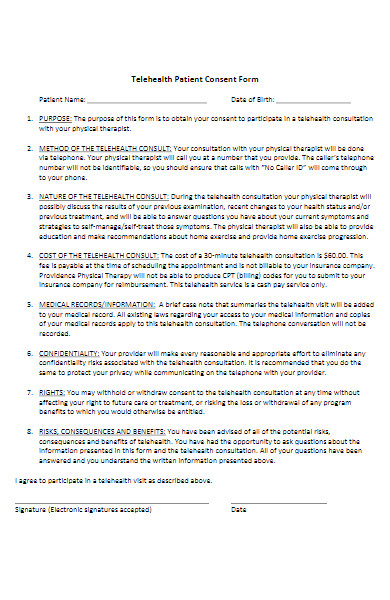
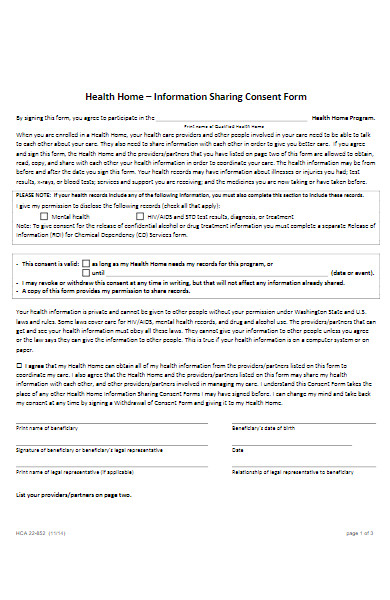
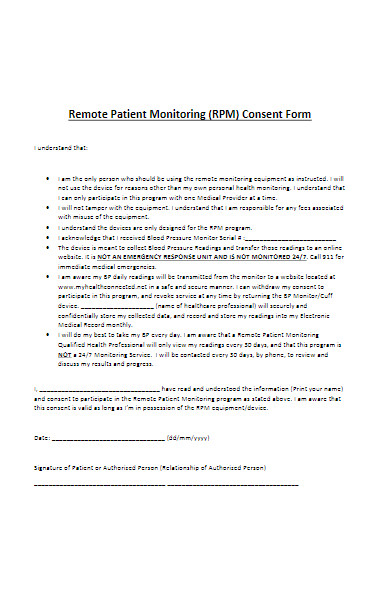
8. Telemedicine Consent Form
- Purpose: For obtaining consent to engage in telehealth or telemedicine services.
- Key Elements: Explanation of telemedicine, privacy considerations, technological requirements, and potential limitations.
9. Psychological Treatment Consent Form
- Purpose: To acquire consent for psychological therapies and treatments.
- Key Elements: Treatment details, risks, benefits, confidentiality, and rights of the patient.
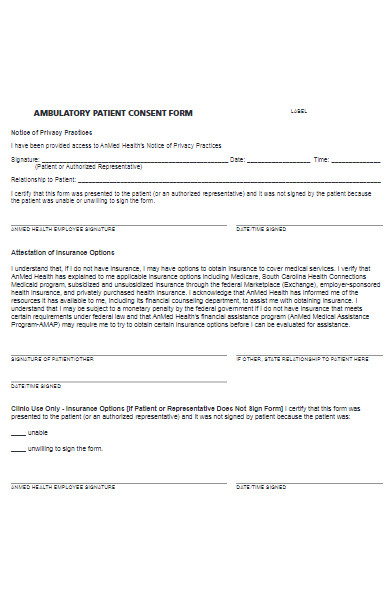
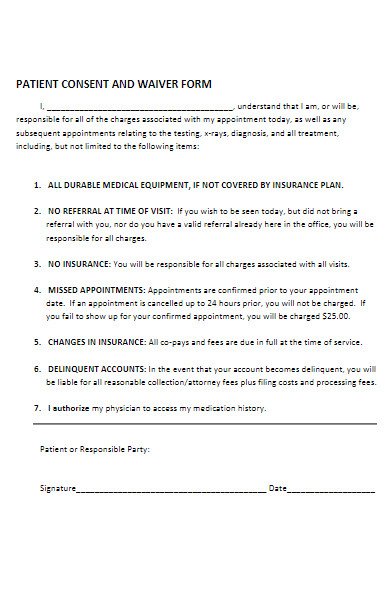
10. Financial Responsibility Consent Form
- Purpose: To ensure that the patient or the patient’s guardian understands and agrees to the financial responsibilities related to the medical services provided.
- Key Elements: Treatment costs, payment expectations, and insurance claim details.
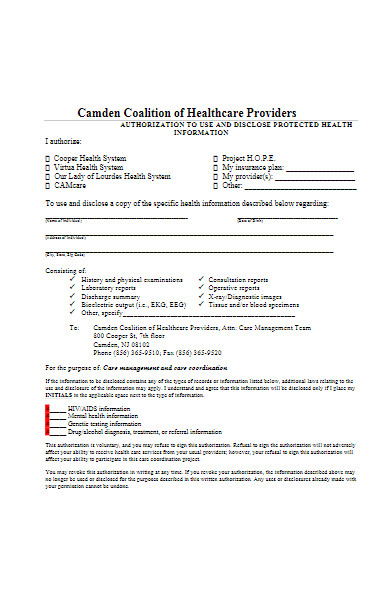
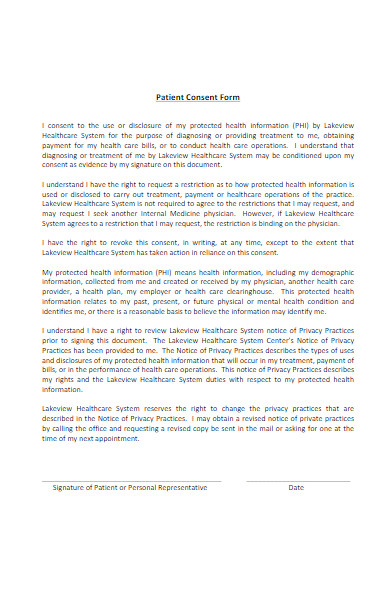
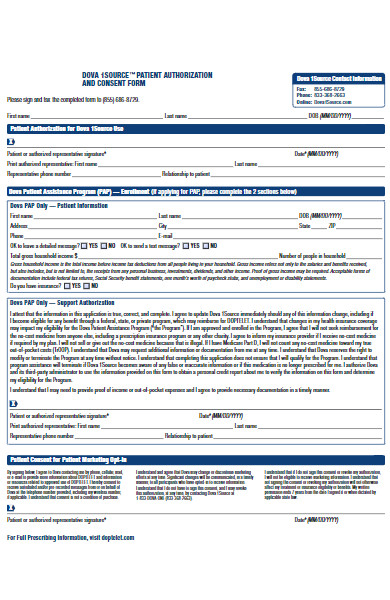
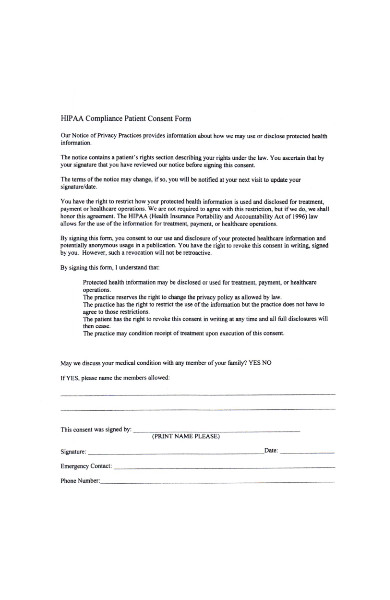
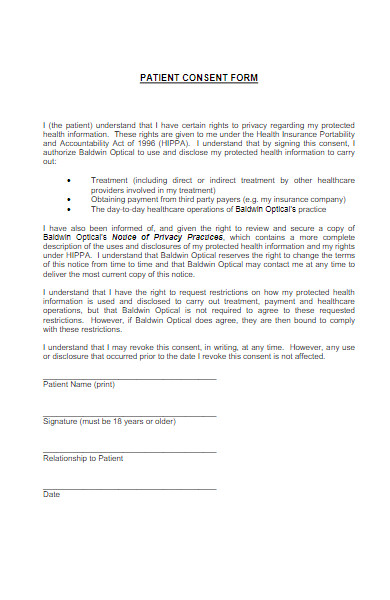
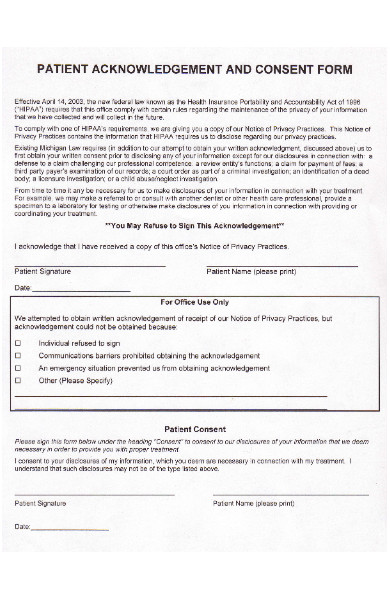
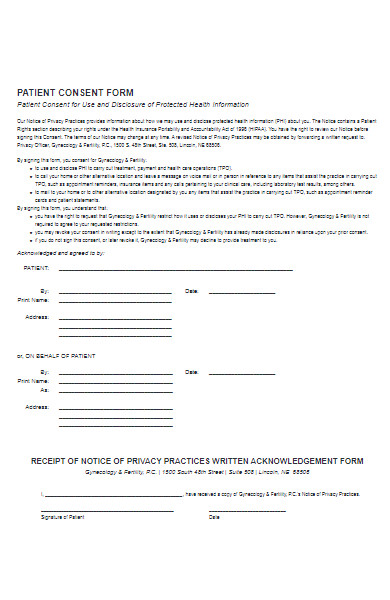
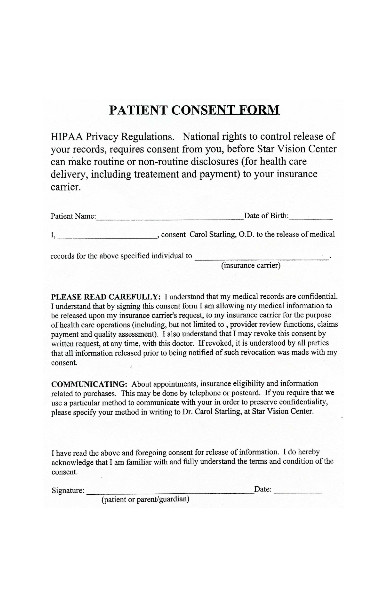
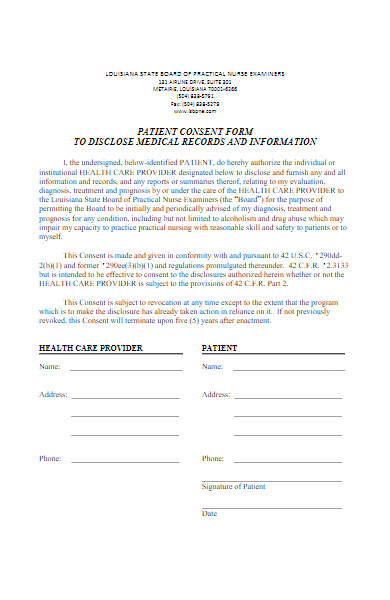
11. HIPAA Consent Form (U.S. Specific)
- Purpose: To ensure understanding and agreement regarding the use and disclosure of patient information as per the Health Insurance Portability and Accountability Act.
- Key Elements: Description of how personal health information may be used and disclosed.
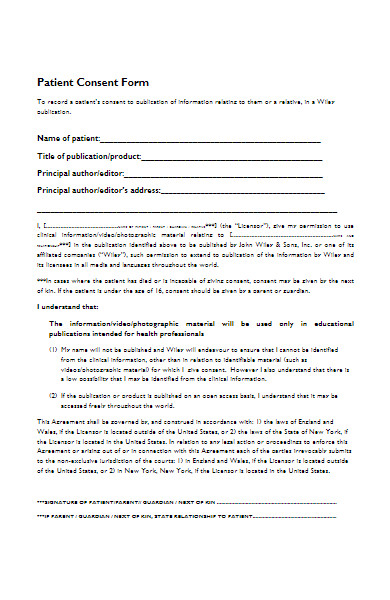
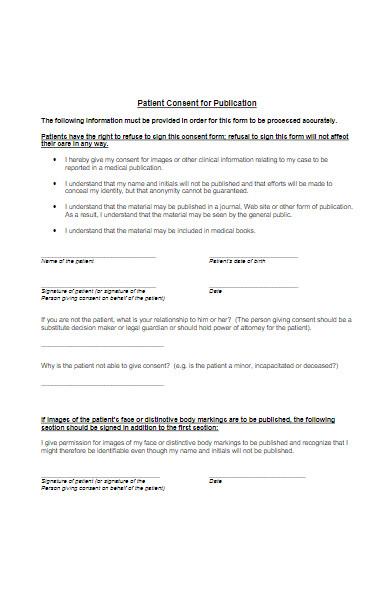
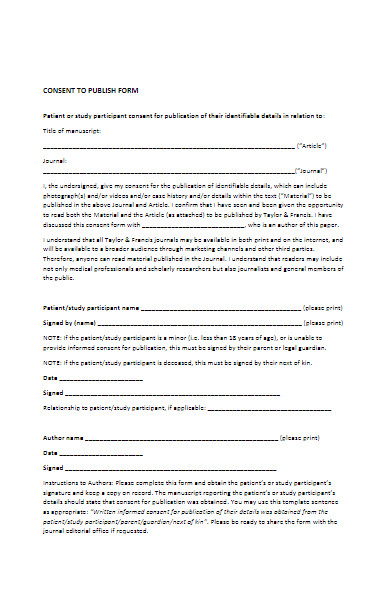
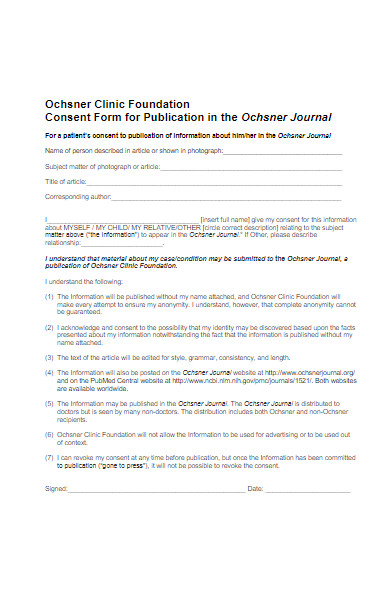
12. Photo and Video Consent Form
- Purpose: To obtain permission for using a patient’s images for educational, promotional, or research purposes.
- Key Elements: Usage details, duration, and the patient’s rights to revoke consent.
Different situations and regions might have specific consent forms that cater to local laws and cultural norms. Always ensure consent forms are compliant with local regulations and ethical standards.
What is the primary purpose of a Patient Consent Form?
The primary purpose of a Patient Consent Form is to ensure that patients are provided with all the necessary information about a medical procedure, treatment, or participation in research in a comprehensive and understandable manner, thus enabling them to make informed and voluntary decisions about their health and medical care. The key objectives include:
1. Ensuring Informed Decisions:
- Informing the Patient: Providing thorough information about the procedure, including benefits, risks, alternatives, and potential outcomes.
- Clarifying Doubts: Offering an opportunity for the patient to ask questions and receive satisfactory answers.
2. Legal and Ethical Compliance:
- Upholding Patient Autonomy: Respecting the patient’s right to make decisions about their own body and health.
- Protecting Practitioners: Serving as a legal document that confirms the patient has been informed and has consented, thereby safeguarding healthcare providers against legal consequences.
3. Establishing Transparency and Trust:
- Building Trust: Demonstrating that the healthcare team values transparency and the patient’s rights, thereby fostering a trusting relationship.
- Verifying Understanding: Ensuring that the patient comprehends all aspects of the intended medical action, reaffirming transparency in the healthcare process.
4. Documenting Consent:
- Recording Agreement: Keeping a documented record that the patient has received all relevant information and agrees to proceed.
- Providing a Reference: Enabling both healthcare providers and patients to refer back to the consent if needed in the future.
5. Facilitating Patient-Centered Care:
- Aligning with Patient Values: Ensuring that the proposed medical intervention aligns with the patient’s values and wishes.
- Promoting Collaboration: Encouraging a collaborative approach towards health management between the patient and healthcare provider.
6. Addressing Privacy and Confidentiality:
- Securing Data: Outlining how the patient’s data will be utilized, stored, and who it will be shared with, ensuring privacy and confidentiality.
- Detailing Data Usage: Describing if, and how, patient data might be used in research, education, or other auxiliary purposes.
In essence, a Patient Consent Form serves as a cornerstone for ethical and patient-centered care, ensuring that the patient’s autonomy is respected and legal standards are upheld, all while establishing a transparent and trustworthy relationship between patients and healthcare providers.
What specific information should a Patient Consent Form include?
A Patient Consent Form should be meticulous, clear, and comprehensive, ensuring it conveys all necessary information and safeguards both the patient and healthcare providers. Here are the specific elements that should be incorporated into a Patient Consent Form:
1. Patient Information:
- Full name
- Date of birth
- Contact details
2. Detailed Procedure Information:
- Name and description of the procedure or treatment
- Objective of the procedure
- Steps involved in the procedure
3. Risks and Benefits:
- Potential risks and complications
- Anticipated benefits
- Probability of success and failure
4. Alternatives to the Proposed Procedure:
- Other available options
- Risks and benefits of alternatives
5. Anesthesia Information (if applicable):
- Type of anesthesia to be used
- Potential risks associated with anesthesia
6. Privacy and Confidentiality:
- How the patient’s information will be used and protected
- Any potential sharing of medical data and for what purpose
7. Financial Information:
- Cost of the procedure
- Payment methods and plans
- Insurance claim details
8. Provider Details:
- Name and credentials of the primary healthcare provider
- Information about other team members (if applicable)
9. Consequences of Non-Treatment:
- What could happen if the patient opts out of the procedure
- Impact on health and quality of life
10. Post-Procedure Information:
- Expected recovery process and duration
- Potential lifestyle changes post-procedure
- Follow-up appointments and care
11. Consent Statement:
- A clear statement where the patient affirms they understand and agree to the procedure
- Space for the patient’s signature and date
12. Withdrawal of Consent:
- Explanation that consent can be withdrawn at any time
- Procedures for withdrawal of consent
13. Legal Guardian or Representative (if applicable):
- Details of the guardian or representative providing consent on behalf of the patient
- Relationship to the patient
14. Witness Details:
- Name, signature, and date from a witness verifying that the consent was willingly given
15. Additional Provisions:
- Any extra local, legal, or institutional requirements
- Special conditions or considerations pertinent to the procedure
The language used should be clear and easily understood by the patient, avoiding excessive medical jargon. Additionally, a space should be provided for the patient to ask questions to ensure absolute clarity and comfort in providing consent. Always ensure that the form adheres to legal and ethical guidelines pertinent to the healthcare setting’s location.
Is it mandatory for all patients to sign a Consent Form before any treatment or procedure?
Yes, obtaining a signed consent form is generally considered mandatory before conducting a treatment or procedure in many healthcare contexts. This practice adheres to the principle of patient autonomy and is a fundamental ethical and legal requirement in healthcare.
Significance of Consent Forms:
- Legal Protection: It safeguards healthcare providers and institutions against legal liabilities and claims related to non-disclosure of information, and unauthorized treatments or procedures.
- Patient Rights: It ensures that the patient’s right to receive information and make autonomous decisions about their healthcare is respected.
- Ethical Practice: It adheres to the ethical norms of medical and healthcare practice, respecting patient dignity and autonomy.
Scenarios and Considerations:
- Emergencies: In certain emergency situations where the patient is unable to provide consent (due to unconsciousness or severe impairment), and waiting might pose a risk to their life or health, healthcare providers might proceed without obtaining formal consent, depending on jurisdictional laws.
- Incompetence: For patients deemed incompetent to make their own healthcare decisions (e.g., certain mental health patients, or individuals with cognitive impairments), consent might be obtained from a legally authorized representative.
- Minors: The consent for treatment for minors (underage individuals) is typically provided by parents or legal guardians. However, the age of consent and rules regarding minor’s consent can vary based on regional laws and specific medical situations (like sexual health, mental health, etc.).
- Non-urgent or Elective Procedures: For non-emergency, elective, or optional procedures, obtaining informed consent is pivotal and non-negotiable.
- Routine Care: While informed consent is crucial for procedures, treatments, and interventions, general, and routine care (like physical examinations, standard tests, etc.) might not always necessitate a formal signed consent form but still involve verbal consent and information provision.
- Research Participation: Consent is paramount for participants involved in research, ensuring they are fully informed of the study’s nature, purpose, procedures, risks, and benefits.
It’s important to recognize that consent is not merely about signing a printable form. The essence of informed consent involves comprehensively educating the patient about the procedure, potential risks, alternatives, and benefits, providing them with ample opportunity to ask questions and consider their options, thereby ensuring their decision is made voluntarily and without coercion.
In contexts and healthcare systems worldwide, variations might exist. Therefore, always consider the specific legal and ethical guidelines applicable to the geographical and institutional context of practice.
Can a patient refuse to sign a Consent Form and what are the implications of doing so?
Absolutely, a patient has the right to refuse to sign a Consent Form, adhering to the principle of autonomy in healthcare. This principle emphasizes that individuals have the right to make informed decisions about their own health and body. A patient may decline a recommended treatment or procedure, even if their decision may result in harm or death.
Implications of Refusing to Sign a Consent Form:
For the Patient:
- Health Risks: Refusal might expose the patient to health risks, especially if the procedure is critical for their well-being.
- Alternative Treatments: The healthcare team may explore other treatment options that are more acceptable to the patient.
- Patient Education: The healthcare provider might engage in further dialogue to ensure the patient fully understands the implications of refusing treatment.
- Respect for Decision: Even after refusal, the healthcare team should respect the patient’s decision and continue to offer necessary support and care.
For Healthcare Providers:
- Legal Protection: Documenting the patient’s refusal to consent safeguards healthcare providers against potential legal implications related to not performing the procedure.
- Ethical Practice: Providers must respect the patient’s autonomy while balancing the principle of beneficence (acting in the patient’s best interest).
- Continued Care: Providers must continue to offer care, even if it’s in a different form or if the patient has refused a particular treatment.
- Patient-Provider Relationship: It’s vital to maintain a positive and respectful relationship with the patient, even amidst disagreements regarding treatment approaches.
Legal and Ethical Aspects:
- Documentation: Even if a patient refuses to sign a consent form, this decision should be documented thoroughly to acknowledge respect for patient autonomy and to have a clear record of the patient’s wishes.
- Informed Refusal: Ensure that the patient’s refusal is informed, meaning they comprehensively understand the potential consequences of not proceeding with the recommended treatment or procedure.
- Second Opinion: Depending on the situation, healthcare providers might suggest obtaining a second opinion to ensure the patient is making a well-rounded decision.
- Treatment of Minors: The refusal of consent by parents or guardians for the treatment of minors can be complex and might necessitate legal intervention if it is deemed that the refusal might cause significant harm or is not in the best interest of the child.
Always consider cultural, social, and personal factors that might influence a patient’s decision to refuse treatment. Engage in open, non-judgmental communication to understand their perspective and provide support, ensuring that their healthcare journey is respectful and patient-centered, even amidst treatment refusals.
Are there different types of Patient Consent Forms for varied medical scenarios?
Yes, different types of Patient Consent Forms are utilized across various medical scenarios to ensure that the patient or their legal representative is adequately informed and consents to the proposed medical intervention. Let’s explore some of these types:
1. Informed Consent Form
- Usage: Employed for most medical procedures, treatments, and interventions.
- Purpose: To inform the patient about the risks, benefits, and alternatives of the procedure and to obtain their explicit agreement.
2. Procedure-Specific Consent Form
- Usage: Applied to specific procedures, like surgeries or specific interventions.
- Purpose: To detail the specific risks and expected outcomes related to a particular procedure.
3. Research Consent Form
- Usage: Implemented when enrolling participants for research studies or clinical trials.
- Purpose: To inform participants about the study’s purpose, duration, procedures, risks, benefits, and to assure confidentiality and voluntary participation.
4. Implied Consent Form
- Usage: Often used in routine or non-invasive examinations like physical exams.
- Purpose: Sometimes consent is implied through a patient’s actions (like extending an arm for a blood test), but documentation is still crucial.
5. Express Consent Form
- Usage: When verbal or non-verbal (written) consent is needed for minor interventions or routine care.
- Purpose: To document the patient’s clear and unmistakable consent to a proposed intervention.
6. Pediatric Consent Form
- Usage: When treating minors.
- Purpose: To secure consent from parents or guardians and sometimes assent from the child, depending on their age and comprehension.
7. Emergency Consent Form
- Usage: In emergent situations where immediate action is needed, and the patient cannot provide consent.
- Purpose: This might involve obtaining consent from next of kin or following specific legal and ethical guidelines for emergency care.
8. Telemedicine Consent Form
- Usage: For engaging in telehealth consultations.
- Purpose: To inform the patient about the nature, benefits, and limitations of telemedicine and to obtain their agreement to proceed.
9. Dental Consent Form
- Usage: Before undergoing dental procedures.
- Purpose: To acknowledge risks and approve proceeding with dental treatments or surgeries.
10. Mental Health Treatment Consent Form
- Usage: Utilized in scenarios involving mental health interventions.
- Purpose: To ensure the patient, or their legal guardian, understands and agrees to the proposed mental health treatment plan.
11. Blood Transfusion Consent Form
- Usage: When a blood transfusion is proposed.
- Purpose: To inform about the benefits and risks like allergic reactions, and to document the patient’s approval or refusal.
12. Anesthesia Consent Form
- Usage: Prior to administering anesthesia.
- Purpose: To ensure the patient understands the risks and agrees to the use of anesthesia during procedures.
Different medical scenarios necessitate tailored consent forms that cater to the specificities and potential risks of varied treatments, procedures, and contexts. Consistently, these forms should elucidate relevant information transparently, ensuring patients can make well-informed decisions about their healthcare journey. Always prioritize clear communication, empathy, and patient-centered care while navigating through the consent process.Our Surgical Consent forms is also worth a look at
How to Create a Patient Consent Form?
Creating a patient consent form involves various steps to ensure it is comprehensive, lawful, and ethically sound. Here’s a step-by-step guide:
Step 1: Understand the Legal and Ethical Implications
- Familiarize yourself with the legal and ethical requirements related to patient consent in your jurisdiction.
- Consider consulting with a healthcare attorney to ensure compliance with laws and regulations.
Step 2: Define the Purpose Clearly
- Explicitly state the purpose of the form and the specific procedure or treatment it pertains to.
- Detail the scope of consent, ensuring it is specific to the procedure, treatment, or research.
Step 3: Explain the Procedure or Treatment
- Detail the procedure/treatment, including what the patient can expect before, during, and after.
- Provide information on the healthcare professionals involved in the procedure or treatment.
Step 4: Detail Risks, Benefits, and Alternatives
- Clearly outline the potential risks and expected benefits of the procedure or treatment.
- Include available alternative procedures or treatments, along with their respective risks and benefits.
Step 5: Outline the Rights of the Patient
- Specify the patient’s right to withdraw consent at any time without impacting their subsequent care.
- Assure the patient of confidentiality and explain circumstances under which information may be shared.
Step 6: Include Space for Questions and Acknowledgments
- Ensure there’s space for the patient to jot down questions during the consent discussion.
- Include statements for the patient to acknowledge that they understand the information and had the opportunity to ask questions.
Step 7: Consent to Procedure and Participant Details
- Have a clear statement where the patient or legal representative consents to the procedure/treatment.
- Include spaces for the patient’s name, date, signature, and details of the legal representative (if applicable).
Step 8: Healthcare Provider Confirmation
- Include a section for healthcare professionals to confirm that they have explained all necessary information and addressed the patient’s questions.
- Include spaces for the healthcare provider’s name, signature, and date.
Step 9: Include a Witness Section (if applicable)
- Some jurisdictions may require a witness to attest that the patient has signed the form voluntarily and with understanding.
- Include spaces for the witness’s name, signature, and date.
Step 10: Validation and Storage
- Ensure the form is stored securely, maintaining privacy and confidentiality.
- Consider creating a digital version to streamline the process and secure storage.
Step 11: Review and Update Regularly
- Periodically review and update the consent form to reflect any changes in procedures, treatments, or legal requirements.
Creating a patient consent form necessitates meticulous attention to detail, ensuring that legal, ethical, and informational aspects are comprehensively covered. Always prioritize patient comprehension, autonomy, and rights while crafting and implementing consent forms in healthcare settings.
Tips for creating an Effective Patient Consent Form
Crafting an effective Patient Consent Form demands a mix of clarity, comprehensiveness, and compliance with legal norms. Here are some tips to enhance the efficacy and reliability of your Patient Consent Form:
1. Prioritize Clarity and Simplicity:
- Use simple, clear language that is easily understood by a layperson.
- Avoid medical jargon; if necessary, provide explanations or definitions.
2. Include All Vital Information:
- Clearly define the procedure, treatment, or intervention, ensuring the scope is easy to comprehend.
- Mention potential risks, benefits, and alternative options available to the patient.
3. Ensure Legal and Ethical Compliance:
- Adhere to legal standards and guidelines related to patient consent in your jurisdiction.
- Consider seeking legal advice to ensure the form’s compliance with healthcare laws and regulations.
4. Be Transparent About Risks and Benefits:
- Honestly communicate all possible risks and benefits related to the procedure.
- Ensure that no aspect of the procedure is hidden or minimized.
5. Facilitate Withdrawal of Consent:
- Include clear instructions and implications regarding the withdrawal of consent.
- Provide an easy-to-follow procedure for revoking consent if the patient chooses to do so.
6. Uphold Patient Privacy:
- Ensure that the form abides by privacy laws like HIPAA (or relevant local laws) in handling patient data.
- Outline how patient information will be used and safeguarded.
7. Specify Details about Participation:
- If applicable, detail how and why a patient is participating in a procedure, trial, or study.
- Make sure to clearly express that participation is voluntary.
8. Ensure Accessibility:
- Make the form accessible in various formats, catering to individuals with disabilities.
- Offer translations in different languages to accommodate non-native English speakers.
9. Involve the Patient:
- Allow space for patients to jot down their questions or concerns.
- Ensure that patients have ample time to read, understand, and ask questions before signing.
10. Provide Contact Information:
- Offer detailed contact information for personnel who can answer questions or provide further clarifications.
- Ensure that a qualified professional is available to respond to queries or concerns.
11. Implement a Review Process:
- Regularly review and update the consent form to incorporate changes in medical practices and legal norms.
- Engage healthcare professionals in the review process to ensure medical accuracy and relevance.
12. Include Confirmation of Understanding:
- Incorporate a section where the patient acknowledges understanding the information provided and consents willingly.
- Consider adding a brief questionnaire to ensure the patient comprehends the key aspects of the consent.
An effective Patient Consent Form is transparent, comprehensive, and patient-centric. It acknowledges the patient’s rights and autonomy, ensuring they are fully informed and comfortable with their consent, bolstering ethical and legal adherence in medical practices.
Patient Consent Forms serve as pivotal legal and ethical tools in healthcare, safeguarding patient autonomy and practitioners alike. They encapsulate clear, comprehensible information about medical procedures, inherent risks, and alternative pathways. Constructing these forms necessitates a blend of legal adherence, ethical compliance, and patient-centered communication, ensuring informed, voluntary, and competent patient participation in their healthcare journey. Crafting and comprehending these forms wisely ensure an ethically sound healthcare framework. In addition, you should review our Dental Consent Form.
Related Posts
-
Landlord Consent Form
-
Passport Consent Form
-
Minor Travel Consent Form
-
Research Informed Consent Form
-
Surgical Consent Form
-
Field Trip Consent Form
-
Tattoo Consent Form
-
FREE 10+ Check Consent Forms in PDF | Ms Word
-
Parental Consent Form
-
FREE 6+ Model Consent Forms in MS Word | PDF
-
FREE 7+ Participant Consent Forms in MS Word | PDF
-
FREE 7+ Therapy Consent Forms in MS Word | PDF
-
FREE 11+ Media Consent Forms in PDF | Ms Word | Excel
-
FREE 22+ Medical Consent Forms in PDF | Ms Word
-
FREE 8+ Participant Consent Forms in PDF | MS Word