A HIPAA Consent Form is a crucial document, intricately designed to safeguard patient health information while ensuring compliance with the Health Insurance Portability and Accountability Act. Navigating through its meaning, exploring various types, examining tangible examples, and comprehending the meticulous creation process are pivotal in enhancing healthcare service integrity. Dive into this comprehensive guide that not only demystifies HIPAA Consent Forms but also imparts invaluable tips to fortify your knowledge and application in the healthcare domain.
What is a HIPAA Consent Form? – Definition
A HIPAA Consent Form is a document used in the healthcare industry to obtain authorization to use or disclose a patient’s protected health information (PHI). These printable form adheres to the regulations set forth by the Health Insurance Portability and Accountability Act (HIPAA), ensuring that any disclosure is in compliance with U.S. law, safeguarding the patient’s privacy and ensuring their health information is protected while enabling necessary data sharing among healthcare providers.
What is the Meaning of HIPAA Consent Form?
The meaning of a HIPAA Consent Form centers around the lawful use and disclosure of a patient’s protected health information (PHI) under the guidelines of the Health Insurance Portability and Accountability Act (HIPAA). This form signifies that the patient, or their legal representative, has been informed of how their health information will be used and has agreed to it being shared for specified purposes, such as treatment, payment, or healthcare operations, thereby ensuring the safeguarding of their privacy and data security.
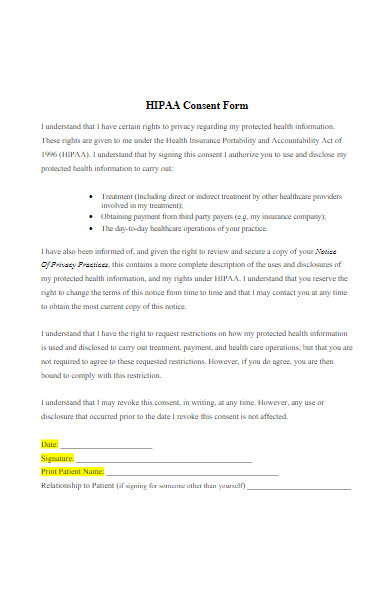
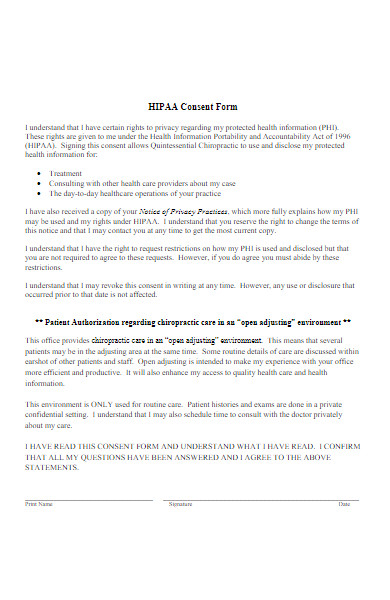
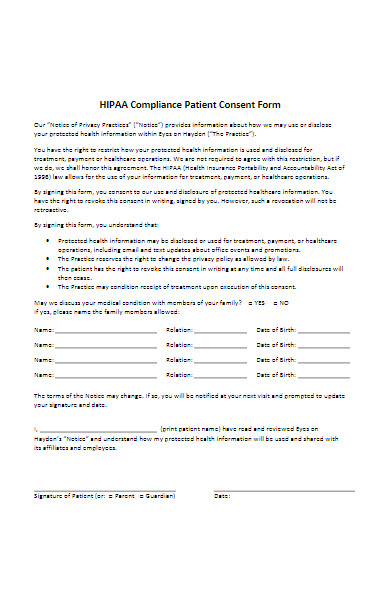
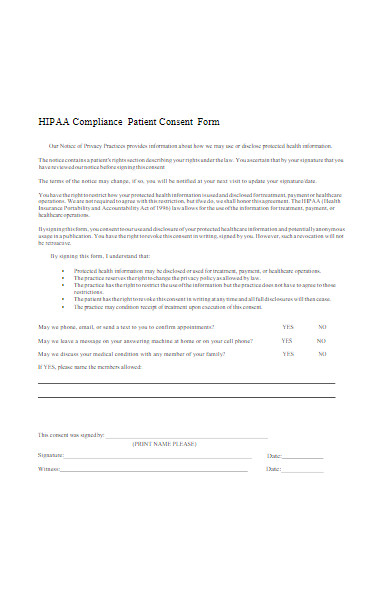
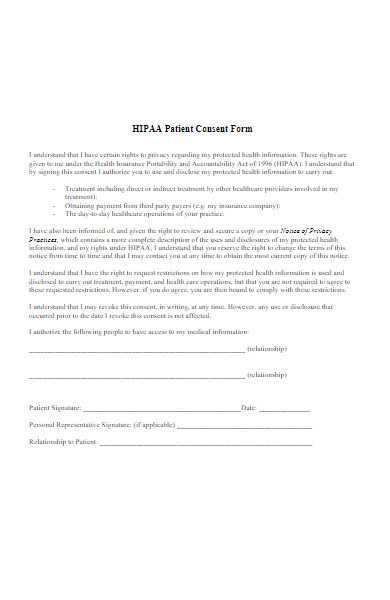
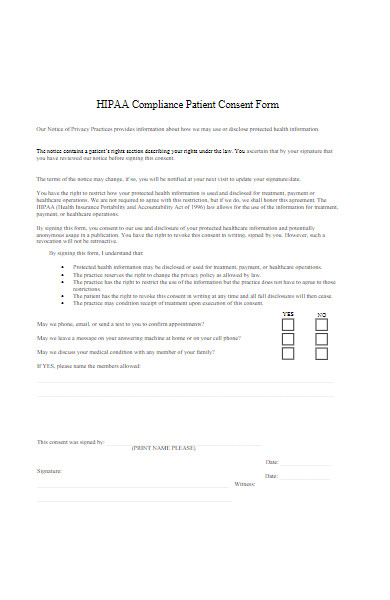
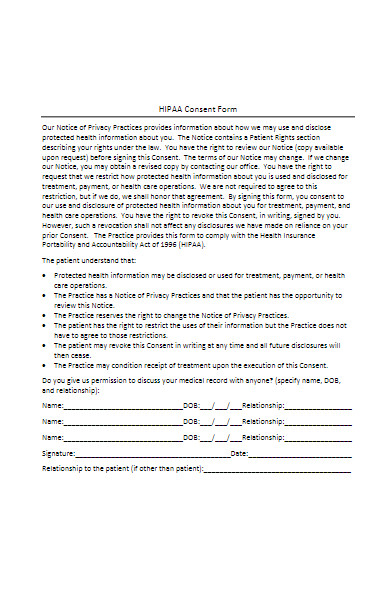
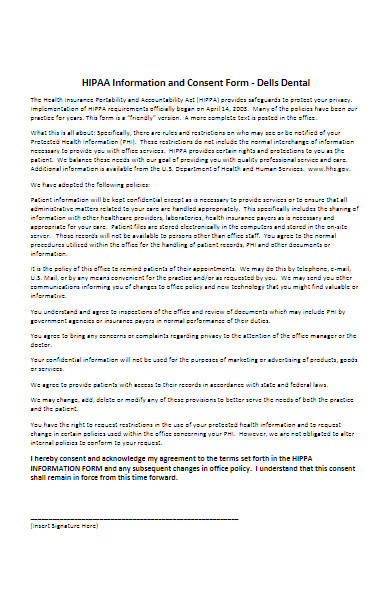
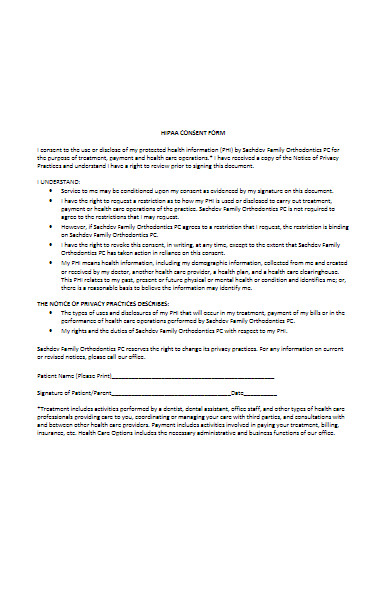
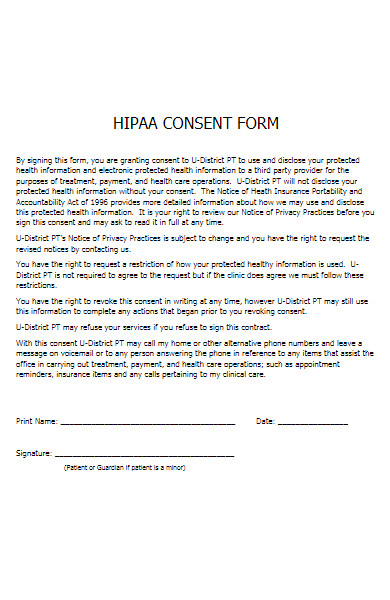
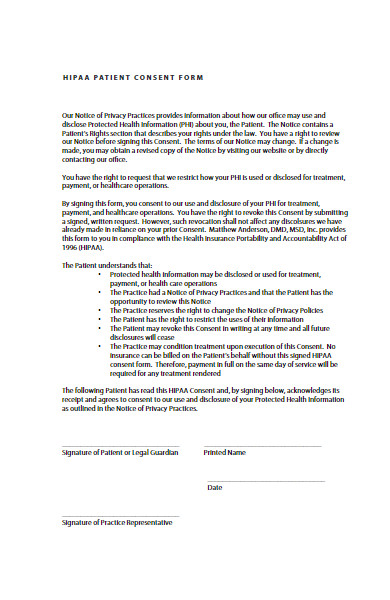
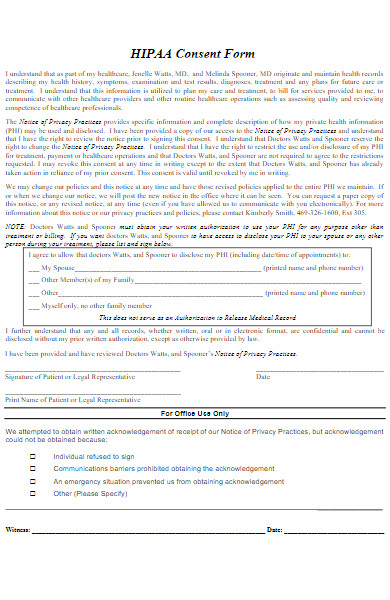
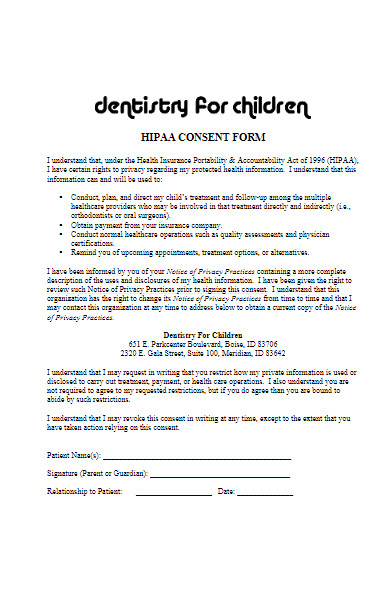
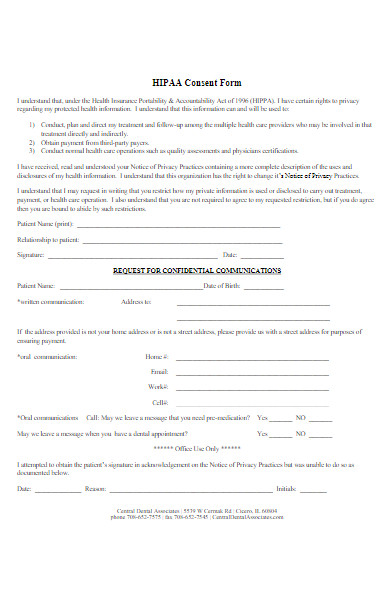
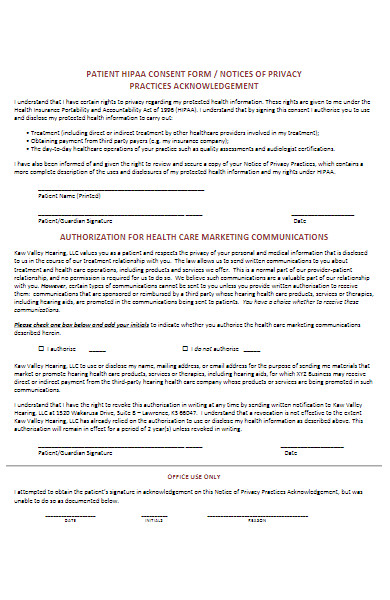
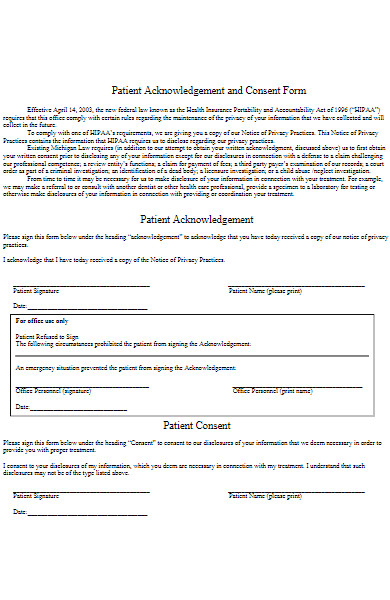
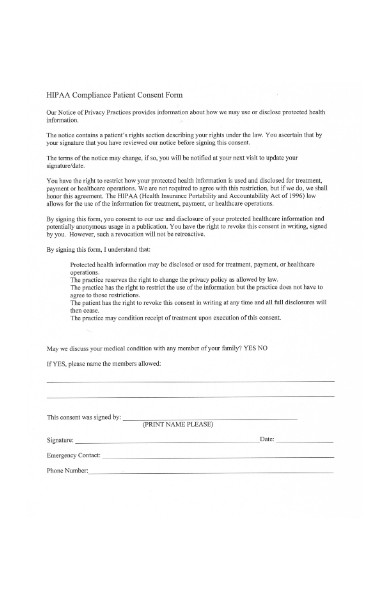
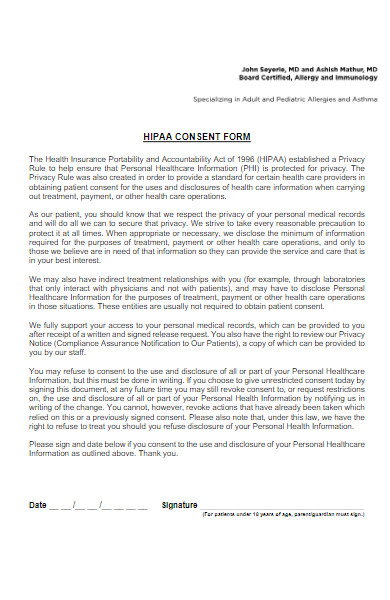
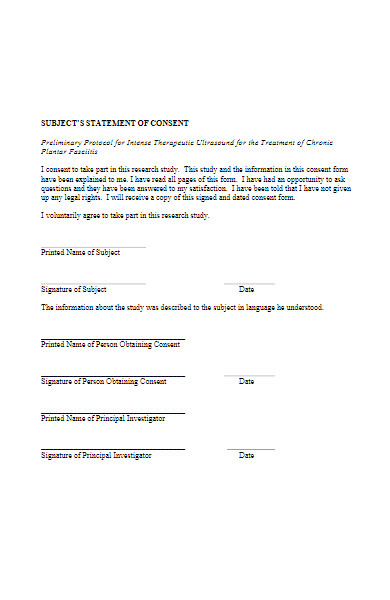
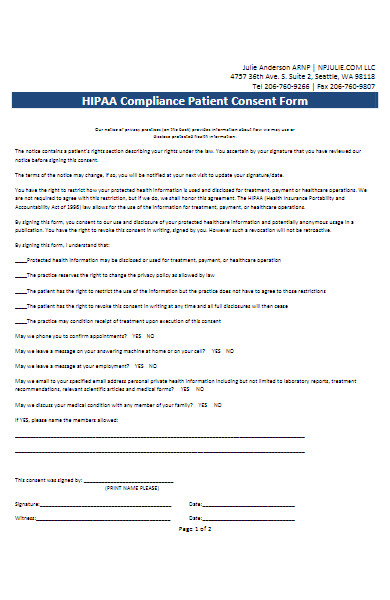
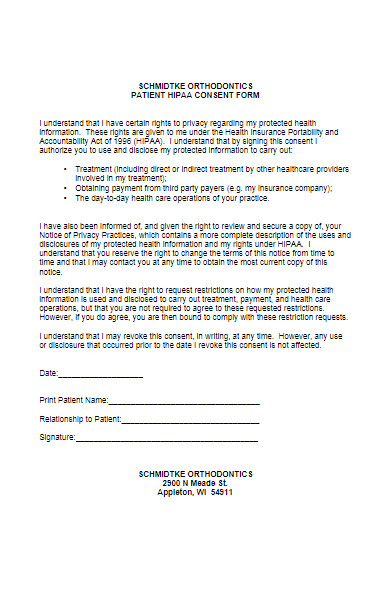
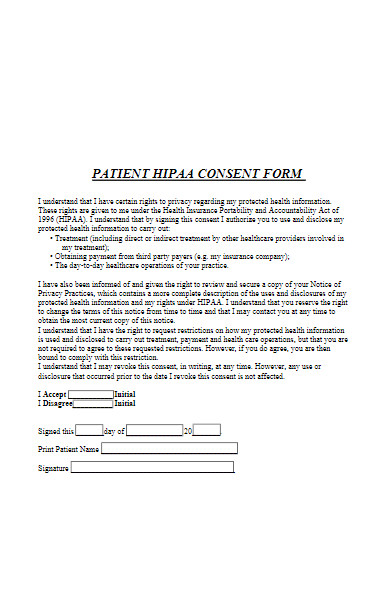
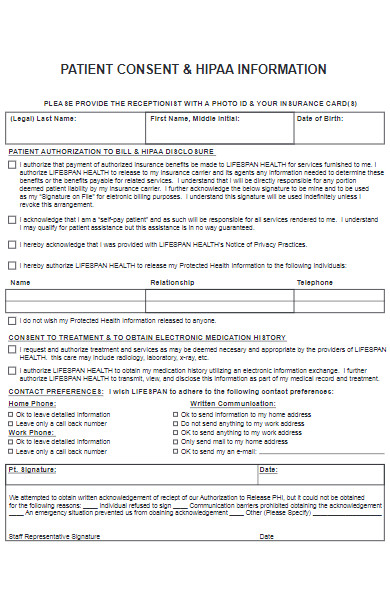
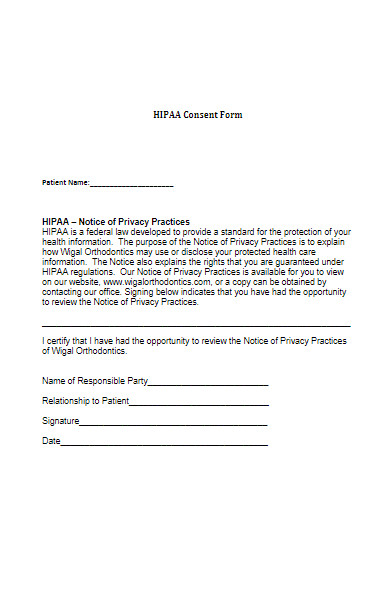
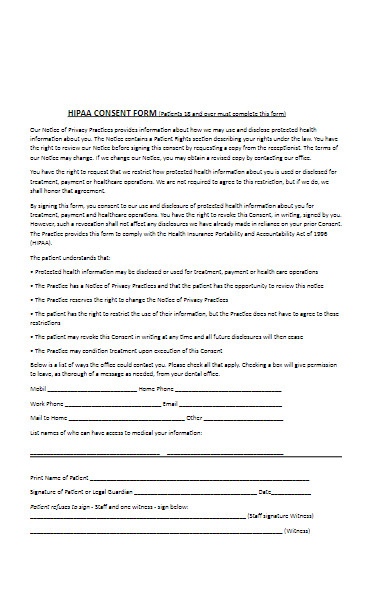
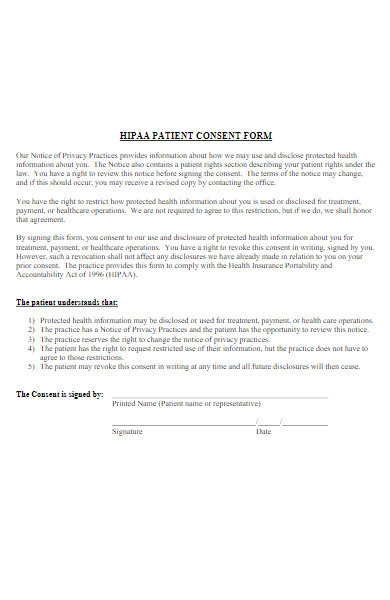
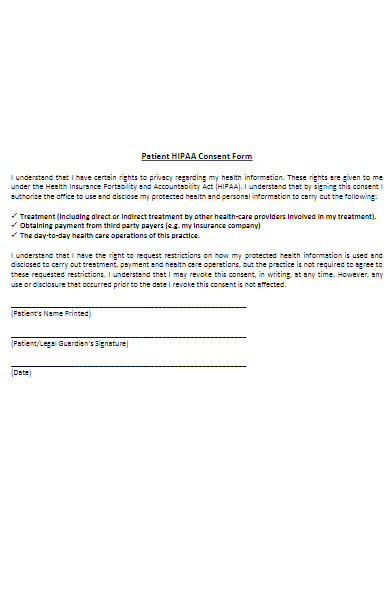
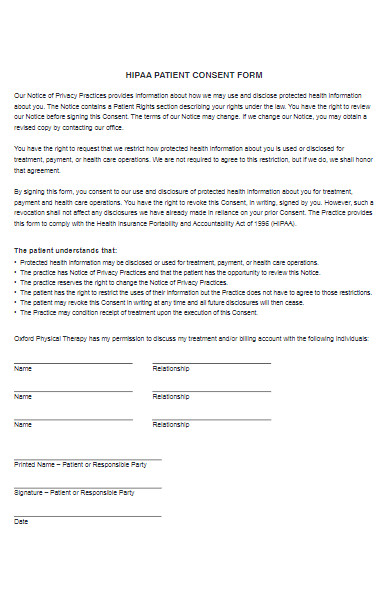
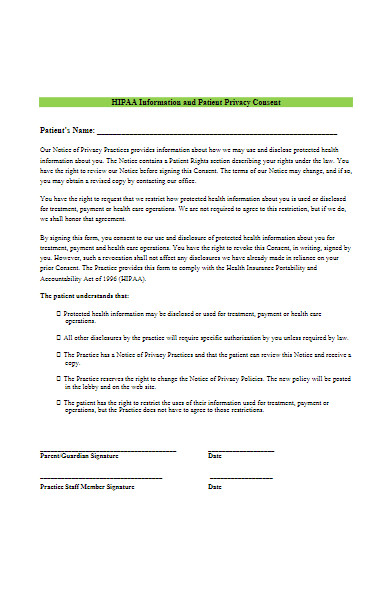
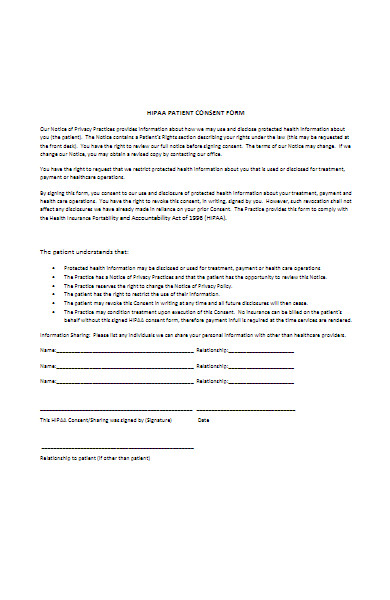
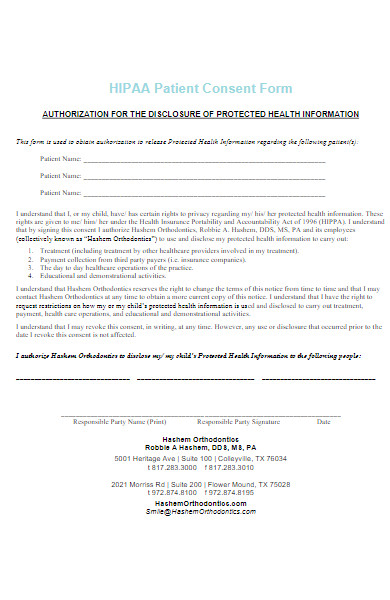
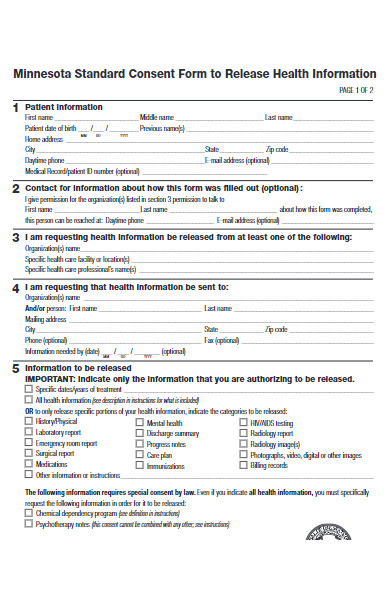
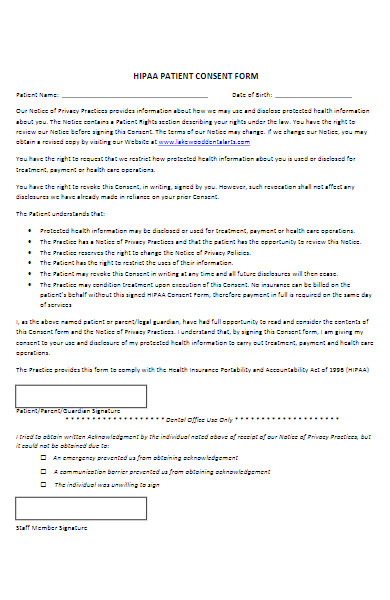
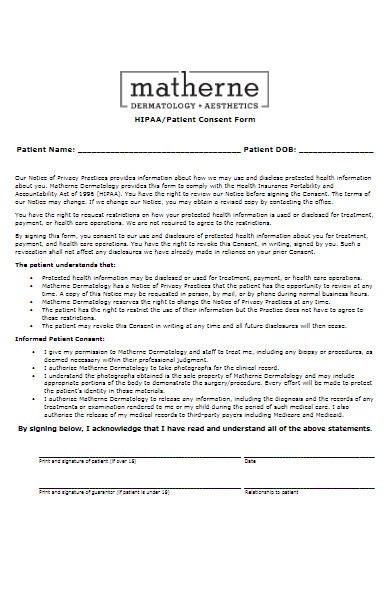
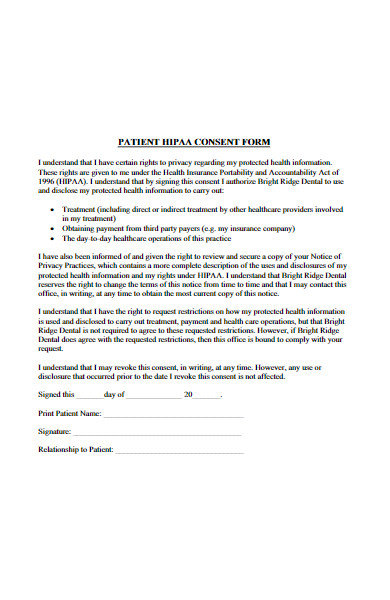
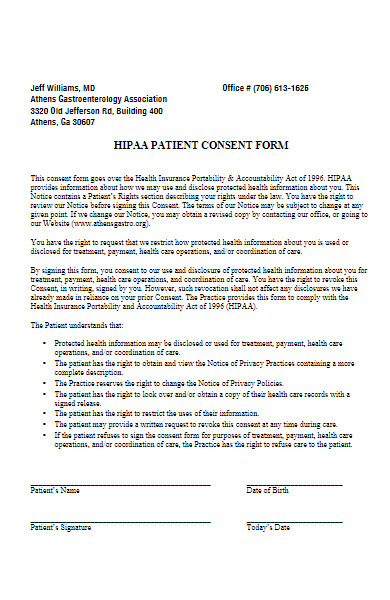
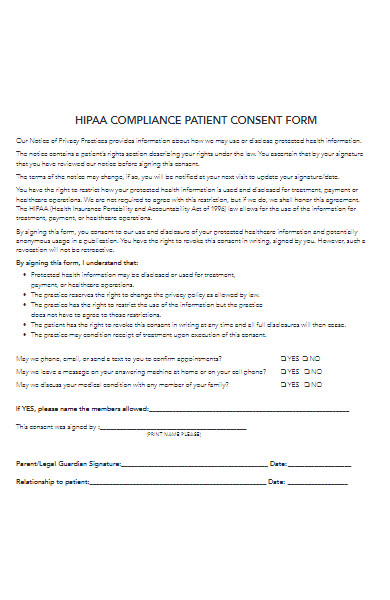
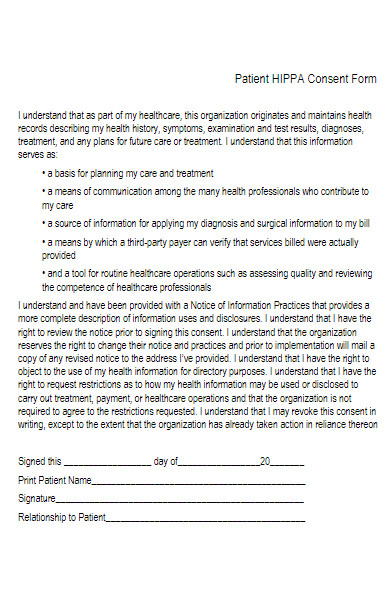
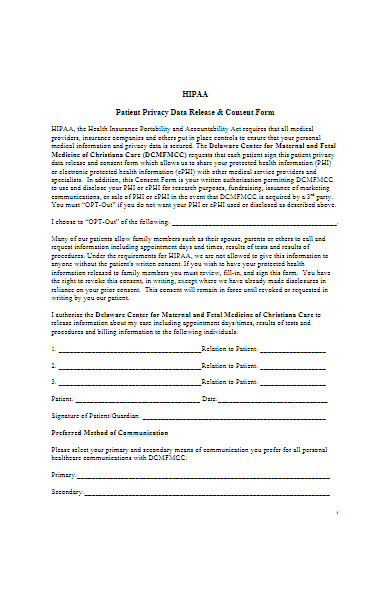
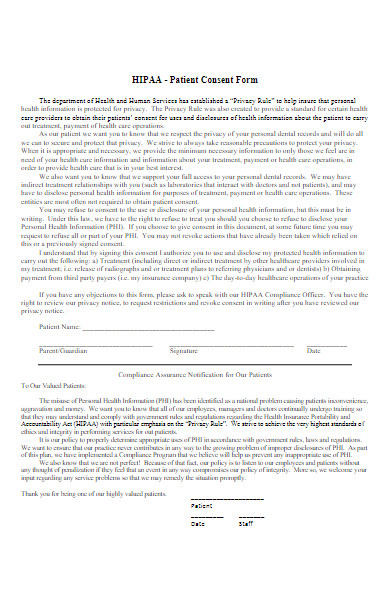
What is the Best Sample HIPAA Consent Form?
A well-structured HIPAA Consent Form ensures the legal and secure use and sharing of protected health information (PHI). A good sample would typically include the following elements:
- Patient Information:
- Full Name
- Date of Birth
- Address
- Purpose of Disclosure:
- Clear statement indicating whether the PHI will be used for treatment, payment, healthcare operations, or another HIPAA-permitted use.
- Information to be Disclosed:
- Detailed list of the types of information to be shared, e.g., medical history, treatment records, etc.
- Name and Information of the Entity Receiving the PHI:
- Name
- Address
- Contact Details
- Expiration Date:
- A specific date or event that signals the end of the consent.
- Patient’s Rights:
- Statement explaining the rights to revoke consent, how to do so, and any exceptions to the right to revoke.
- Signature Block:
- Space for the patient or their representative to sign and date the form.
- A relationship to the patient if signed by a representative.
- Notice of Privacy Practices Acknowledgement:
- Statement confirming the patient has received a copy of the Notice of Privacy Practices.
- Additional State-specific Requirements:
- Depending on jurisdiction, there may be additional elements or alternative requirements.
Having a thorough, well-formatted HIPAA Consent Form that patients can easily understand, and that aligns with legal requirements, is paramount in maintaining compliance and ensuring secure PHI handling. Note: Always consult with a legal or compliance professional when creating or updating forms to ensure they meet all current regulatory requirements.
FREE 50+ HIPAA Consent Forms in PDF
51. Children HIPAA Patient Consent Form
What makes a form HIPAA compliant?
A HIPAA-compliant form adheres to the regulations set by the Health Insurance Portability and Accountability Act (HIPAA) of the United States, ensuring the safeguarding of protected health information (PHI). Here are several key elements that make a form HIPAA compliant:
1. Data Protection:
- Encryption: PHI transmitted over networks should be encrypted to prevent unauthorized access.
- Data Integrity: Ensuring that the information remains accurate and consistent during storage and transmission.
2. Access Controls:
- Authentication: Only authorized personnel should have access to PHI.
- Authorization: Different levels of access should be set based on job responsibilities.
3. Audit Controls:
- Monitoring: Constantly monitor and log access and activities related to PHI.
- Audit Trails: Maintain logs to analyze any breaches or unauthorized access.
4. User Identification:
- Unique User IDs: Each user must have a unique identifier for traceability.
- Emergency Access: Establish procedures for obtaining necessary PHI during an emergency.
5. Transmission Security:
- Integrity Controls: Implement security measures to ensure that electronically transmitted PHI is not improperly modified.
- Automatic Logoff: Implement electronic procedures that terminate an electronic session after a pre-determined time of inactivity.
6. Valid Authorization:
- Patient Approval: Obtain patient consent and authorization before using or disclosing their PHI.
- Minimum Necessary: Only the minimum necessary information should be used or disclosed for the intended purpose.
7. Notification and Communication:
- Breach Notification: Notify concerned parties in case of any breach of unsecured PHI.
- Privacy Policies: Clearly outline the policies and procedures for using and disclosing PHI.
8. Data Back-up:
- Storage: Ensure reliable backup and storage of PHI data to prevent data loss.
- Recovery: Implement a plan for retrieving data in case of an emergency or data loss.
9. Employee Training:
- Awareness Programs: Conduct regular training and awareness programs for employees about HIPAA policies and procedures.
- Security Training: Ensure staff are knowledgeable about how to securely manage and handle PHI.
10. Patient Rights:
- Access: Allow patients to have access to their PHI.
- Amendments: Enable patients to request corrections or additions to their PHI.
11. Agreements and Contracts:
- Business Associate Agreements: Ensure that third parties (if involved) comply with HIPAA rules through formal contracts.
12. De-identification:
- Anonymization: Ensure that PHI cannot be traced back to an individual unless necessary.
Implementing these aspects ensures the confidentiality, integrity, and availability of PHI, adhering to the HIPAA regulations and safeguarding against unauthorized access and data breaches.
When is a HIPAA Consent Form Required?
A HIPAA Consent Form is typically required in the United States whenever a healthcare provider, health plan, or a healthcare clearinghouse (referred to as “covered entities”) needs to use or disclose a patient’s Protected Health Information (PHI) for purposes other than treatment, payment, or healthcare operations. Here are specific scenarios in which a HIPAA Consent Form might be required:
1. Disclosure of PHI for Non-Standard Purposes:
- When PHI is to be used or disclosed for purposes not inherently involved in providing healthcare, such as research, marketing, or sale of the PHI.
2. Sharing Information with Third Parties:
- If a healthcare provider wishes to share a patient’s PHI with third-party entities not involved in the patient’s care.
3. Participation in Research:
- When a patient’s PHI is intended to be used in research, even if the information is being shared for research under an Institutional Review Board (IRB) waiver of authorization.
4. Sensitive Information:
- In certain jurisdictions or scenarios, additional consent may be needed for sharing specific types of sensitive information (like mental health, genetic information, or HIV status).
5. Marketing and Fundraising Communications:
- When a covered entity wants to use PHI to communicate with the patient about products, services, or for fundraising activities.
6. Psychotherapy Notes:
- Separate permissions are often required for sharing psychotherapy notes.
7. Minors and Emancipated Individuals:
- Situations involving minors or emancipated individuals might have specific rules for accessing, disclosing, or allowing decision-making related to PHI.
8. Legal and Administrative Requirements:
- In instances where legal and administrative proceedings require the sharing of PHI, adhering to the guidelines is essential.
It is crucial to note that HIPAA allows for the use and disclosure of PHI without a patient’s consent for standard purposes of treatment, payment, and healthcare operations except in particular circumstances or state laws that mandate explicit patient consent. Ensuring that the HIPAA Consent Form is structured according to HIPAA guidelines, ensuring privacy and legal adherence, is pivotal in maintaining compliance and safeguarding patient information.
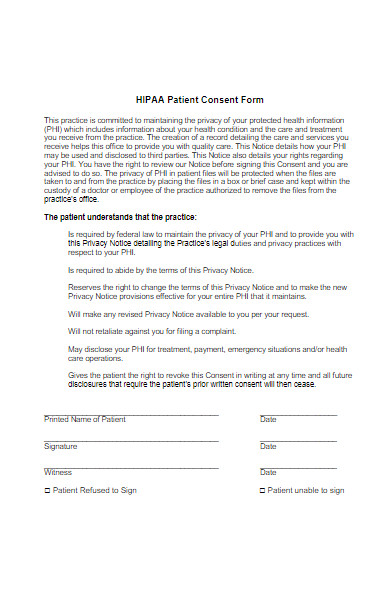
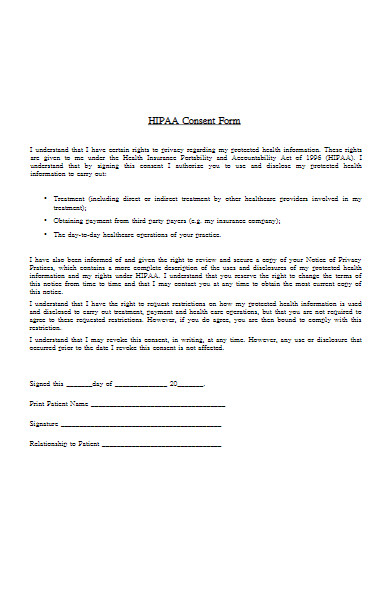
What Information is Included on a HIPAA Consent Form?
A HIPAA Consent Form is pivotal for protecting patient information and ensuring that such data is handled according to HIPAA regulations. Here’s a breakdown of the essential information typically included on a HIPAA Consent Form:
1. Patient Identification:
- Full name.
- Date of birth.
- Contact information.
2. Purpose of Disclosure:
- Clear definition of why the information is being used or shared.
3. Information to be Disclosed:
- Description of the specific data to be used or shared (e.g., medical records, billing information).
4. Identity of the Information Recipient:
- Name and contact details of the person/organization receiving the information.
5. Expiration Date:
- A specific date or event that signals the end of the authorization.
6. Patient’s Rights:
- Right to revoke the authorization.
- Right to receive a copy of the disclosure.
7. Disclosure Statement:
- Acknowledgement that once information is disclosed, the receiver might not be obligated to abide by HIPAA.
8. Signature Block:
- Space for the patient or their representative to sign and date the form.
9. Relationship to the Patient:
- If signed by a representative, define the relationship to the patient and the authority to sign.
10. Optional Information:
- Additional notes or instructions regarding the information disclosure.
11. Entity’s Use and Disclosure Obligations:
- A section that outlines how the entity will use and protect the shared information.
12. Special Information Categories:
- If applicable, separate authorizations for sharing of special information categories like HIV, mental health, or genetic data.
13. Copy Provision:
- Statement ensuring the patient receives a copy of the signed form.
This structure ensures the HIPAA Consent Form is comprehensive, adhering to HIPAA regulations, and safeguarding both patient information and the healthcare entity. It’s crucial that patients understand the form thoroughly, ensuring informed and voluntary consent. Consequently, healthcare entities often take additional steps to explain the form and its implications to the patients before securing their signature.
How to Properly Fill Out a HIPAA Consent Form?
Filling out a HIPAA Consent Form involves careful attention to ensure accuracy and compliance with regulations. Here’s a step-by-step guide on how to properly complete a HIPAA Consent Form:
1. Patient Identification
- Clearly write the patient’s full name, date of birth, and contact details.
2. Detailed Information Disclosure
- Specify the types of information to be disclosed (e.g., medical history, diagnosis).
3. Purpose of Information Use
- Define and describe why the information is being disclosed and used.
4. Recipient Details
- Accurately provide the name and contact details of the entity receiving the information.
5. Expiration Date
- Set a specific expiration date or event that will terminate the authorization.
6. Understand Patient Rights
- Acknowledge the patient’s right to revoke the authorization and how they can do it.
7. Disclosure Notification
- Ensure that the form notifies the patient that the information, once disclosed, may no longer be protected by HIPAA.
8. Signature and Date
- Ensure that the patient (or their authorized representative) signs and dates the form.
9. Relationship to Patient
- If a representative signs the form, indicate their relationship to the patient and the authority for representation.
10. Special Information Disclosure
- If the disclosure involves specific categories of information (e.g., HIV status), ensure that these are clearly defined and consented to.
11. Additional State-Specific Requirements
- Ensure any additional elements as required by the state’s laws are incorporated and filled out (e.g., witness signature).
12. Copy Provision
- Provide the patient with a copy of the signed authorization form.
Notes for Completion:
- Accuracy: Ensure all written information is accurate and legible.
- Voluntary Completion: Ensure that the patient fills out the form voluntarily and without coercion.
- Clarity: Make sure every section of the form is understandable to the patient. Address any questions or concerns before proceeding.
- Privacy: Ensure the form is completed in a private and secure environment to protect the patient’s information.
This detailed step ensures the HIPAA Consent Form is filled out comprehensively and ethically, maintaining the integrity of the information and protecting both the patient and the entity involved. Always remember to check for any updates or changes in HIPAA regulations that may affect the consent process.
Is a Digital Signature on a HIPAA Consent Form Valid?
Yes, a digital signature can be valid on a HIPAA Consent Form if it adheres to the requirements specified by the Health Insurance Portability and Accountability Act (HIPAA) and other applicable laws like the Electronic Signatures in Global and National Commerce Act (ESIGN) and the Uniform Electronic Transactions Act (UETA). These provisions essentially allow electronic signatures to be used in place of handwritten ones, given that certain criteria are met:
Key Considerations for Digital Signatures on a HIPAA Consent Form:
- Authentication:
- The signature must reliably authenticate the signer and validate their identity.
- Integrity:
- The form and signature must be secure and safeguarded against alterations post-signature.
- Intent to Sign:
- The process must demonstrate clear intent by the signer to approve the information and actions.
- Association of Signature:
- The signature and electronic form must be logically associated or linked.
- Audit Trail:
- An audit trail should document when the signature was applied and under what circumstances.
- Accessibility:
- A copy of the signed document must be accessible and reproducible for reference by any entitled party.
- Security:
- The electronic system used to obtain the digital signature must ensure the security and confidentiality of the health information, as per HIPAA regulations.
- Revocation of Consent:
- The process should allow for the withdrawal of consent and ensure that the signer is aware of this right.
- Notification:
- Procedures should be in place to notify and confirm receipt of the electronically signed document.
- Compliance:
- Ensure compliance with any state-specific laws that might have further requirements regarding electronic signatures.
Final Thoughts:
- Legal Counsel: Always consult legal counsel to ensure all aspects of your digital signature process are in compliance with federal and state laws.
- Technology Selection: Choose a technology platform that offers secure, compliant electronic signature capabilities.
- Training: Ensure that all stakeholders, especially the healthcare providers and administrative staff, are adequately trained on the digital signature system to avoid any compliance issues.
In essence, digital signatures on HIPAA Consent Forms can not only be valid but also streamline the consent process, reduce paperwork, and enhance the patient experience, given that all legal and regulatory obligations are meticulously adhered to.
What Should Be Done if a HIPAA Consent Form is Misplaced or Lost?
When a HIPAA Consent Form is misplaced or lost, it constitutes a serious matter as it involves potential unauthorized disclosure of protected health information (PHI). Below are steps and strategies that might be considered in such an incident:
Immediate Actions:
- Inform Key Personnel:
- Notify the privacy officer, legal team, and management immediately about the lost form.
- Documentation:
- Document all relevant details about the incident including when, how, and possibly why the form was lost.
- Investigation:
- Conduct an internal investigation to determine the scope and potential risks of the incident.
Risk Assessment:
- Assess the Risks:
- Evaluate the likelihood of PHI being accessed, used, disclosed, or compromised.
- Individual Impact:
- Assess the level of potential harm to the individual(s) involved if their PHI were disclosed.
Response Strategy:
- Mitigation:
- Develop strategies to mitigate the risks associated with the loss of the form, such as advising individuals on protecting their identity.
- Communication:
- Depending on your risk assessment and applicable laws, notify affected parties and communicate the incident transparently while ensuring not to violate any other compliance standards.
- Regulatory Reporting:
- If the loss of the form is deemed a breach under HIPAA, report it to the Department of Health and Human Services (HHS) and, if necessary, communicate with affected individuals and media outlets as per HIPAA breach notification rules.
Preventive Measures:
- Implement Safeguards:
- Analyze the incident to identify and implement additional safeguards to prevent similar occurrences in the future.
- Training:
- Enhance training programs to reinforce the importance of safeguarding PHI and protocols to follow in handling such forms.
- Audit:
- Perform an audit of current practices to ensure that other forms are not at risk of being lost.
Review and Update Policies:
- Review Policies:
- Evaluate current policies and procedures regarding the handling, storage, and disposal of HIPAA consent forms and PHI.
- Update Procedures:
- If any loopholes or inefficiencies are identified during the review, update policies accordingly to enhance security and compliance.
Legal Consultation:
- Legal Advice:
- Engage with legal counsel to navigate through regulatory compliance, especially in communicating with involved parties and regulatory bodies.
Addressing a misplaced or lost HIPAA Consent Form involves immediate remedial actions, thorough investigation, regulatory compliance, risk mitigation, and implementing robust strategies to prevent future incidents. Each step should be approached with diligence and adherence to HIPAA regulations to safeguard the privacy and well-being of the individuals affected while maintaining regulatory compliance. Always consult with a healthcare compliance professional or legal counsel for precise guidance specific to the incident and jurisdiction.You should also take a look at our HIPPA Form.
Can a HIPAA Consent Form Be Denied by a Patient?
Yes, a patient can deny or refuse to sign a HIPAA consent form. According to the Health Insurance Portability and Accountability Act (HIPAA) in the United States, patients have the right to manage and direct the use of their personal health information (PHI). This means they can choose to deny signing a consent form that allows a healthcare provider or other covered entity to use or disclose their PHI for certain purposes, especially for purposes beyond healthcare provision, payment, and operations.
Implications of Denying HIPAA Consent:
- Limited Sharing of Information:
- Healthcare providers may not share the patient’s health information for purposes like marketing or research.
- Possible Impact on Care:
- While refusing to sign a consent form for disclosure to other purposes does not affect the patient’s treatment, if the form relates to sharing information for treatment purposes, it could limit the healthcare provider’s ability to coordinate care or obtain necessary information from other providers.
- Restrictions:
- Patients can request restrictions on certain uses or disclosures of their PHI.
- Privacy of Information:
- Providers must respect the patient’s wishes not to share information, as long as it adheres to law and policy.
Rights and Protections:
- Patient Rights:
- Patients have rights over their health information, including the right to obtain a copy and correct inaccuracies.
- Provider Protections:
- Healthcare providers must adhere to HIPAA regulations which provide protections against unauthorized uses or disclosures of PHI.
- Special Scenarios:
- There might be situations, like cases involving public health or law enforcement, where the provider can disclose PHI even without the patient’s consent, as stipulated under HIPAA.
Considerations for Healthcare Providers:
- Communication:
- Clearly communicate to the patient the implications of not signing the consent form.
- Documentation:
- Document any refusal thoroughly to ensure clarity and protect against potential legal implications.
- Alternative Approaches:
- Explore alternative ways to achieve healthcare objectives while respecting the patient’s privacy choices.
- Legal & Ethical Obligations:
- Always align actions and policies with ethical standards and legal obligations.
While patients have the right to refuse to sign a HIPAA consent form, healthcare providers should navigate such situations with clear communication, understanding, and adherence to ethical and legal guidelines. Balancing the patient’s privacy rights while ensuring quality care and compliance with regulations is imperative. Always consult legal counsel for specific advice related to HIPAA compliance and managing patient consents and refusals effectively.
Is There a Standard Format for a HIPAA Consent Form?
Yes, while there is not a single standard format for a HIPAA consent form due to the varying needs and contexts of different healthcare providers, there are certain key elements that are generally included to ensure compliance with the Health Insurance Portability and Accountability Act (HIPAA) regulations:
Key Elements of a HIPAA Consent Form:
- Patient Identification:
- Full name, date of birth, and other relevant identifying information.
- Purpose of Information Use or Disclosure:
- Clearly state the purpose behind collecting and sharing the patient’s personal health information (PHI).
- Specific Information to be Used or Disclosed:
- Detail the specific types of PHI that will be used or shared.
- Name or Identification of the Person/Entity to Disclose Information:
- Specify who is authorized to make the disclosed, whether it’s a particular doctor, specialist, or healthcare facility.
- Name or Identification of the Person/Entity Receiving the Information:
- Identify who will receive and possibly utilize the PHI.
- Expiration Date or Event:
- Define the period during which the consent is valid, or detail the event after which the consent is no longer applicable.
- Patient’s Right to Revoke Consent:
- Explicitly mention that the patient has the right to revoke their consent at any time and explain the procedure for doing so.
- Potential for Redisclosure Information:
- Notify that once the PHI is disclosed, it may no longer be protected under HIPAA and might be redisclosed.
- Signature and Date:
- Ensure space for the patient (or a representative) to sign and date the form, confirming their understanding and consent.
- Additional State-Specific Information:
- Depending on the state, additional information or clauses may be required.
Additional Considerations:
- Clarity and Language:
- Make sure that the form is written in clear, understandable language to ensure the patient fully comprehends what they are consenting to.
- Language Options:
- In areas with diverse populations, consider providing the form in multiple languages.
- Electronic Consent:
- Ensure that electronic consent forms are also in compliance with HIPAA regulations, and are as valid as their paper counterparts.
- Legal Review:
- Have legal professionals review the form to ensure it adheres to both federal and state laws and regulations.
Creating a HIPAA consent form should be done with careful consideration and a thorough understanding of HIPAA regulations. It is recommended to consult with a healthcare attorney or a professional experienced in healthcare compliance to ensure that the fillable form adequately protects the patient’s rights and the healthcare provider’s interests and that it adheres to all applicable laws.
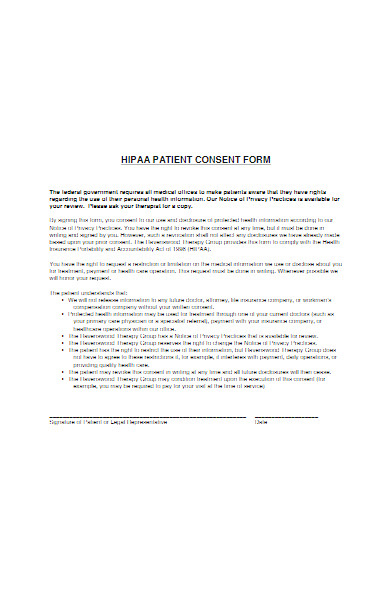
How to Create an HIPAA Consent Form ?
Step 1: Understand HIPAA Requirements
- Familiarize yourself with the HIPAA Privacy Rule, which protects patients’ health information.
- Make sure to know the specific information that must be disclosed and the conditions under which disclosures of health information may be made.
Step 2: Gather Necessary Information
- Compile all the information that needs to be incorporated into the consent form, such as patient identification, purpose of information use, and specifics about the information to be disclosed.
Step 3: Draft the Consent Form
Include Key Components:
- Patient Identification: Name, DOB, and contact details.
- Purpose of Disclosure: Clearly define why the PHI is being used or disclosed.
- Information to be Disclosed: Specify which aspects of PHI will be disclosed.
- Disclosure Entities: Detail who will disclose and receive the PHI.
- Expiration: Mention when the authorization expires.
- Revocation Rights: Describe how patients can revoke their consent.
Step 4: Include Legal Statements
- Provide a statement about the patient’s right to revoke their authorization.
- If the disclosure impacts the patient’s treatment or payment, make this clear on the form.
Step 5: Make it User-Friendly
- Ensure the language is clear and easily understood by the general public.
- Consider incorporating headings, bullet points, and bold text for easy reading.
Step 6: Ensure Accessibility
- Consider creating forms in multiple languages based on your patient demographics.
- Make sure the form is available in both physical and digital formats for ease of use.
Step 7: Implement a Storage System
- Decide on a secure method to store the filled forms, ensuring that they’re easily retrievable when needed.
Step 8: Legal & Compliance Review
- Have the drafted form reviewed by a legal professional to ensure all elements are compliant with HIPAA and state laws.
Step 9: Train Staff
- Ensure that all staff members are adequately trained on when and how to utilize the HIPAA consent form.
Step 10: Periodical Review
- Regularly review and update the form as per any updates in laws or organizational practices.
Step 11: Patient Communication
- Make sure to communicate effectively with patients regarding the purpose and importance of the consent form.
Step 12: Establish a Retrieval and Response System
- Ensure that once forms are submitted, there’s a system in place for timely processing and responding to any requests or revocations.
Creating an HIPAA consent form requires a meticulous understanding of legal requirements and an organized implementation process. Regularly revisiting and updating the form and associated processes will help in maintaining compliance and safeguarding patient information. Always consider professional advice for accurate and legal form creation and management.
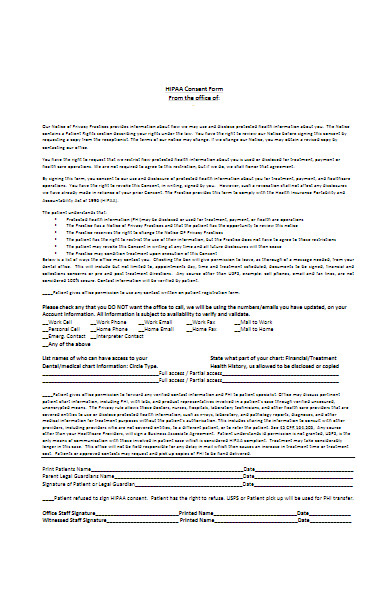
Tips for creating an Effective HIPAA Consent Form
Creating an effective HIPAA Consent Form is pivotal to ensure both compliance with regulations and clarity for patients. Below are some tips to craft an effective HIPAA Consent Form:
1. Maintain Clarity
- Simple Language: Use clear and straightforward language to ensure comprehension by all patients.
- Explicit Detailing: Be explicit about the usage of the data, entities involved, and patient rights.
2. Ensure Compliance
- Adherence to Law: Make sure your form adheres to HIPAA regulations and any relevant state laws.
- Legal Review: Have a legal professional or compliance expert review the form.
3. Provide Detailed Information
- Data Usage: Explain precisely why and how the patient’s data will be used.
- Revocation Right: Inform patients about their right to revoke consent and the process to do so.
4. User-Friendly Design
- Legible Font: Use a readable font size and style.
- Organized Layout: Ensure the layout is organized and logically sequenced.
- Accessible Formats: Provide the form in formats accessible to individuals with disabilities.
5. Specify Disclosure
- Entities Involved: Clearly list who will be disclosing and receiving the information.
- Type of Information: Specify the type of information being shared.
6. Mention Timeframes
- Effective Period: Clearly state how long the consent will be valid.
- Deadline Information: Include any relevant deadlines for consent revocation or data sharing.
7. Incorporate Languages
- Multilingual Options: Offer forms in different languages prevalent among your patient demographic.
8. Integrate Digital Platforms
- Electronic Signatures: Ensure your form can accept electronic signatures.
- Online Accessibility: Make the form accessible and submittable online if possible.
9. Protect Privacy
- Confidentiality Assurance: Assure patients that their information will be kept confidential and secure.
- Data Security: Implement strong data security measures for both physical and digital forms.
10. Implement a Review System
- Periodic Updates: Regularly review and update the form for compliance and practicality.
- Feedback Mechanism: Allow space for feedback to understand any patient concerns or confusions.
11. Facilitate Ease of Use
- Guidance: Provide a guide or assistance in filling out the form when required.
- Availability: Ensure forms are easily available both in physical formats and online.
12. Offer Copies
- Providing Records: Give patients a copy of the signed form for their records.
13. Staff Training
- Effective Communication: Train staff to explain and assist with the form effectively.
- Process Understanding: Ensure staff understands the importance and process related to the form.
14. Regular Auditing
- Ensure Compliance: Periodically audit processes to ensure ongoing compliance and efficacy.
- Update as Needed: Make necessary changes based on audit findings and feedback.
Crafting an effective HIPAA Consent Form is a delicate balance of maintaining legal compliance while ensuring ease of understanding and use for the patients. Always approach with a patient-centric mindset, ensuring that their rights, understanding, and ease are at the forefront of design and implementation.
Navigating through the intricacies of HIPAA Consent Forms requires a detailed understanding of its meaning, diverse types, and adhering to stringent legal frameworks. This guide elucidates the foundational knowledge, provides tangible examples, and steers you through a methodical creation process, ensuring your form is both compliant and transparent. Adopting these insights will streamline patient communication and safeguard your practice against potential non-compliance pitfalls. In addition, you should review our Research Consent forms.
Related Posts Here
-
Informed Consent Form
-
Minor Travel Consent Form
-
Field Trip Consent Form
-
12+ Photo Consent Form
-
FREE 8+ Botox Consent Forms in PDF | MS Word
-
FREE 8+ Dental Consent Forms in PDF | MS Word
-
FREE 7+ Sample Privacy Consent Forms in PDF | MS Word
-
FREE 6+ Sample Child Travel Consent Forms in PDF | MS Word
-
FREE 50+ Patient Consent Forms Download – How to Create Guide, Tips
-
FREE 30+ Piercing Consent Forms Download – How to Create Guide, Tips
-
FREE 50+ Background Check Consent Forms Download – How to Create Guide, Tips
-
FREE 35+ Service Consent Forms Download – How to Create Guide, Tips
-
FREE 2+ Consent to Appropriation of Name Forms in PDF
-
FREE 7+ Sample Consent to Treat Forms in PDF | MS Word
-
FREE 11+ Sample Parental Consent Forms in PDF | MS Word